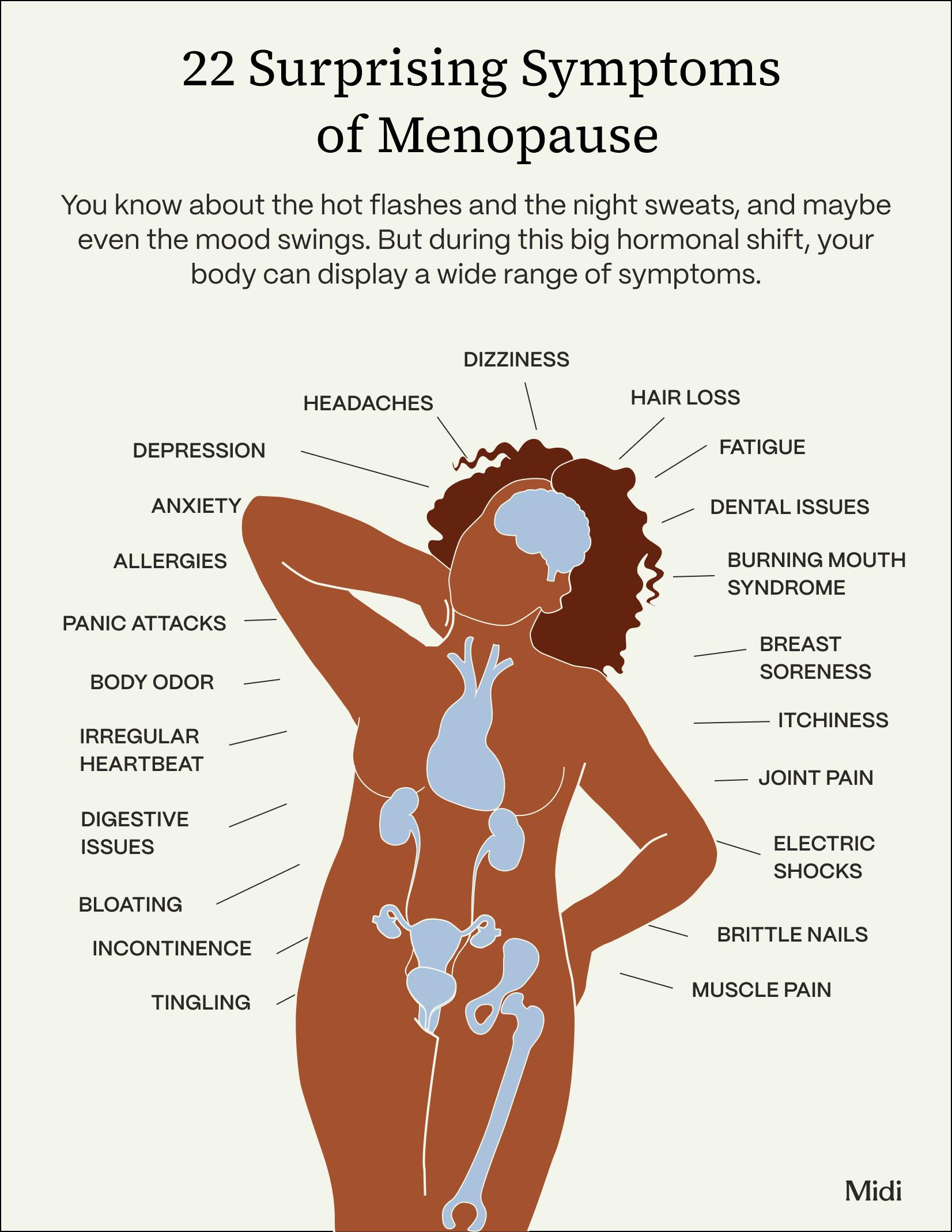
Menopause brings more than just hot flashes—it can come with surprising symptoms that affect your hair, teeth, skin, nails, and even brain function. As estrogen levels decline, you might notice changes in unexpected areas of your health. Menopause specialists can help you develop a personalized care plan to tackle these symptoms and take control of your health.
When it comes to menopause, knowledge is power and relief. The more you understand about the symptoms you’re experiencing, the faster you can take steps toward feeling better, with the help of a Midi clinician or another specialist in hormone transition.
But the only symptom pretty much every woman knows about is hot flashes. There are many more common symptoms during the hormone transition, which begins with perimenopause, usually in your mid-forties.
Then there are the ones most women, and lots of doctors, have no clue about. We’re talking about allergies, dental problems, changes in body odor and dozens more. When we stay in the dark about “unusual” menopausal symptoms—which aren’t so unusual at all—they go undiagnosed, leading to frustration and unnecessary days of feeling “off,” or worse. That needs to change, for you and for all of us, because when women thrive, the world thrives with them.
As you explore the 22 (yes, 22!) surprising symptoms below, remember that you’re not alone if you’re dealing with any of them, and all can be improved or resolved with the right support.
1. Can Menopause Cause Breast Soreness?
Similar to breast soreness some women get during their period, about a third of women experience it during the menopausal transition. This time around, it can worsen as hormones surge and drop more erratically. You may even feel a burning sensation, along with general tenderness.
What helps:
- Over-the-counter pain medications
- Supplements such as vitamin E and B
- Switching your bra to a more supportive, comfy option.
2. Does Menopause Cause Itching?
Some women report feeling unusual itchiness during the menopause transition, and according to the The North American Menopause Society, it can strike the face, back, chest, genital area—pretty much anywhere. Why does this happen? Estrogen helps to keep skin healthy by supporting the production of collagen and natural oils, as well as retaining moisture. Through the hormone transition, estrogen steadily declines, which means drier, thinner, and for plenty of women, itchier skin.
Dryness continues post menopause, but the itchy sensation usually subsides. In the meantime, up your skincare game to improve this symptom and reap extra anti-aging benefits.
What helps:
- Slathering on sunscreen and moisturizer
- Scratching as little as you can
- Discussing the issue with your dermatologist and/or gynecologist
3. Does Menopause Cause Tingling?
A strange crawling sensation, numbness, or pins and needles in your extremities (hands, feet, arms, legs) can be a symptom of menopause. Also known as paresthesia, the odd feeling typically lasts for a few minutes at a time.
Once again, estrogen fluctuations, which impact the central nervous system, are the root cause here. When estrogen levels stabilize, the tingling fades away.
What helps:
- Maintaining a healthy diet, exercise and sleep routine
- Salt baths, and magnesium supplements
- Medications such as anticonvulsants
- Hormone replacement therapy
4. Menopause & Dental Health
Falling estrogen levels contribute to loss of bone density, which may lead to osteoporosis. Like any other bone, your jaw can become weaker, raising your risk of gum disease, tooth sensitivity, pain, decay and even loose or lost teeth.
What helps:
- Good dental hygiene
- Regular dentist check-ups
- Hormone replacement therapy
5. Can Menopause Cause Joint pain?
Estrogen helps to reduce inflammation, regulate fluid levels, and protect bones—and all those benefits keep joint pain at bay. As levels decline during the menopausal transition, achiness in your knees, shoulders, neck, elbows and hands might crop up.
More than half of women in this life stage suffer from aches, stiffness, and swelling, and symptoms are usually worse in the morning when joints are particularly stiff.
What helps:
- Everyday movement, especially strength training like push ups, squats, and lifting weights
- Yoga, which builds both strength and flexibility
- Eating plenty of anti-inflammatory foods
- Supplements such as magnesium
6. Menopause & Muscle Pain
While muscle pain is a normal part of aging (add it to the list), menopause can make it worse. In fact, 56% of menopausal women report tight, tender, or strained muscles. The backstory? Estrogen helps to balance cortisol, aka the stress hormone, in your body, so when estrogen levels waver and drop, cortisol can rise. Spiking cortisol often leads to tight, tense muscles.
What helps:
- Getting the sleep and rest you need
- Paying attention to your posture and alignment
- Hormone replacement therapy
7. Burning Mouth Syndrome during Menopause
Imagine the sensation when you take a sip of too-hot coffee—that’s pretty much what burning mouth syndrome (BMS) feels like. The scalding, tingling feeling may affect the gums, lips and cheeks.
What helps:
- Cognitive behavior therapy, stress management, meditation and yoga
- Medications used to treat neurological disorders, including anxiety and depression
8. Electric Shocks During Menopause
What could cause a short, sharp jolt, like having a rubber band snapped against your skin? It’s estrogen again. Because the hormone affects the nervous system and cardiovascular function, fluctuating levels can cause neurons to misfire. Women who experience electric shock sensations often feel them before a hot flash, and they can be as painful as they sound.
What helps:
- Finding ways to manage stress, starting with mindfulness and meditation
- Cutting back on alcohol, a potential trigger
9. Menopause Bloating
That unpleasant feeling of fullness or tightness in your abdomen could be hormone-related, particularly during perimenopause, when hormone levels swing wildly. High levels of estrogen may cause your body to retain water, and things aren’t much better when estrogen levels are low, because that decreases bile production, resulting in constipation, gas and bloating which can hang around for just a few hours, or several days.
About 60% of women complain of bloating during the menopausal transition, but know that after menopause, that full, puffy feeling is likely to diminish.
What helps:
- A diet low in salt and sugar
- Managing stress
- Exercising regularly
10. Menopause and Digestive Issues
Digestive health patterns change during the menopausal transition for some women, bringing a range of problems including constipation, looser bowel movements, gas, and stomach pain. For those already diagnosed with irritable bowel syndrome, digestive problems might get worse during perimenopause.
What helps:
- Focusing on your microbiome—the vast ecosystem of beneficial microbes located in your intestinal tract. Generally healthy eating (lots of veggies and fruit is rule #1) and gradually adding more fiber to your diet helps to feed these “good bugs.”
- Adding phytoestrogens such as soy, oats and barley to your diet.
11. Does Menopause Cause Thinning Hair or Hair Loss?
Noticeable hair loss—shedding more than 125 hairs per day, thinning hair in certain areas only, or a generally less active growing phase—are all associated with menopause. About 50% of all menopausal women and around 80% of postmenopausal women experience hair loss, and for many, it’s a blow to self-image and confidence .
Lowered estrogen triggers an increase of androgen, a male hormone. That can mean less hair on the head along with fuzzy hair in new areas (the chin is prime territory). While this is a progressive condition, treatment can help hair loss from worsening.
What helps:
- A well-balanced diet rich in vitamins
- Taking supplements, including Vitamin D and Collagen
- Reducing stress and finding healthy coping mechanisms
- Oral medications such as minoxidil and spironolactone
12. Does Menopause Cause Brittle Nails?
Changes in your nails (they’re drier, crack, split and chip away easily, or tend to curl at the ends) are a symptom 30% of women experience in the menopause transition. Why? Because lowered estrogen decreases the strengthening keratin in your nails, as well your body's ability to retain moisture. Both lead to brittleness.
What helps:
- Hydration
- Eating a diet containing lots of whole grains and essential fatty acids
- Avoiding smoking
- Moisturizing hands regularly
13. Menopause and Irregular Heartbeat
Anywhere from 19% to 47% of women experience heart palpitations during the menopause transition, and they can be disconcerting, to say the least. Described as loud, racing, pounding, fluttering or skipping beats, this change in heart rhythm can occur along with dizziness, and may put some at an increased risk of heart and circulatory disease.
Now for the “why”: Several studies show beneficial effects of estrogen on artery walls, blood vessels and cholesterol levels, so when it declines, changes in those areas can trigger palpitations. Your heart rate may increase by 8 to 16 beats per minute, and by much more for some women, pushing all the way to 200 beats per minute.
What helps:
- Exercise bolsters cardiovascular health and helps restore the heart’s natural rhythm, so any activity that doesn’t trigger palpitations will do you good
- Maintaining a healthy weight and eating a healthy diet
- Avoiding smoking
- Hormone replacement therapy
14. Does Menopause Cause Headaches?
A steady estrogen level is ideal for neurologic function, which is why some women experience headaches and migraines during their menstrual cycles, when estrogen dips. Similarly, during perimenopause, erratic hormone levels may trigger headaches. But here’s good news: About 70% of women usually see some improvement after menopause.
What helps:
- Pain medications
- Regular aerobic exercise (research shows it increases nitric oxide which helps relax blood vessel muscles)
- Acupuncture and behavioral therapy that incorporates relaxation and helps you identify and avoid triggers
- Supplements such as magnesium, petasites hybridus, and riboflavin
15. Can Menopause Cause Dizziness?
An estimated 25-35% of women aged 45–60 report “feeling dizzy or faint” at least once a day. Research confirms that dizziness can be related to estrogen deficiency during menopause, as well as bone loss. Another likely cause: Hormonal changes that affect the cardiovascular and nervous system, which can bring on lightheadedness, disorientation, or vertigo. Fatigue stemming from hot flashes and night sweats may only make woozy feelings worse.
What helps:
- Keeping yourself hydrated
- Anti-dizziness and anti-anxiety medications
- Hormone replacement therapy
16. Menopause and Allergies
Do foods and environments that never bothered you in the past now trigger sneezes, hives, acne or something else? As the body deals with numerous changes during menopause, several factors affect the immune system, which responds by over-firing histamines. The result is extra sensitivity to allergens, and women experience new, old, and worse allergy signs and reactions. A recent study examined the link between menopause and new-onset asthma and showed the odds of getting asthma were more than twice as high for women in the menopausal transition compared to non-menopausal women.
What helps:
- Knowing your triggers and reducing exposure
- Taking antihistamines
17. Menopause and Incontinence
About 50% of postmenopausal women suffer from loss of bladder control (say, on the way to the bathroom) or involuntary urinary leakage that may suddenly happen with a sneeze or laugh. All these urinary issues are associated with hormonal changes that lead to loss of elasticity in the vaginal tissue, thinning of the lining of the urethra and weakening of the pelvic floor muscles.
Incontinence problems are common, but women shouldn’t just accept them as a normal part of life.
What helps:
- Exercises that work on the pelvic floor muscles (kegels and other kinds of pelvic floor therapy)
- Cutting back on caffeine and alcohol
- Hormone replacement therapy
18. Menopause and Body Odor
You’re getting the picture on estrogen: This hormone influences pretty much every system in your body, leading to some unexpected symptoms, including body odor. Hormonal shifts during the menopause transition, just like during puberty, cause an increase in sweating and overheating which can make some women smell a little “off.”
Body odor is no cause for medical concern and fairly straightforward, so put away the shame and try some simple fixes.
What helps:
- Dressing in layers
- Experimenting with different, and stronger deodorants
19. Menopause and Fatigue
Tiredness is a tricky symptom, because it has so many potential causes at midlife (family, work, all of it) and may show up in different ways—feeling drained, lacking motivation, or struggling with concentration and problem solving. But hormone fluctuation plays a role, and other symptoms of menopause, especially trouble sleeping and night sweats, only make the problem worse. About 73% of women are affected by fatigue for a span of 8 to 14 years.
What helps:
- Making time for exercise
- Developing a good sleep routine
- Limiting caffeine and alcohol
- Quitting any nicotine habit
20. Can Menopause cause depression?
Unlike garden-variety moodiness, depression is a serious condition that lasts for longer periods of time, and it affects 20% of women going through menopause. In a study published by the Journal of The North American Menopause Society, researcher Ellen W. Freeman, PhD, explains that your mental health history factors into your risk: “Women with a history of depression are nearly five times more likely to have a diagnosis of major depression in the menopausal transition, whereas women with no history of depression are two to four times more likely to report depressed mood compared with premenopausal women.”
Estrogen helps to support “feel good” brain chemicals, such as serotonin and norepinephrine, responsible for mood stabilization, alertness and energy. When estrogen fluctuates and declines, those chemical levels are thrown off along with it, contributing to depression. The positive news? It does not usually follow you past menopause, and most importantly, can be improved—sometimes within days or weeks—with the right support.
What helps:
- Different forms of exercise such as walking, dancing and swimming
- Therapy and professional help
- Prescription medications
- Hormone replacement therapy
21. Menopause and Anxiety
Important but little known fact: As many as 51% of women experience symptoms of anxiety during menopause, some for the first time in their lives. The symptoms are both psychological, described as nervousness, tension, worry and restlessness, and physical, including shaking, heavy breathing, and pounding heart.
One explanation: Estrogen is necessary for the production of serotonin, the brain chemical responsible for leveling mood. When estrogen and progesterone levels rollercoaster during perimenopause, and starts to decline overall, the brain has fewer chemical tools to cope with stressors, which can result in anxiety.
What helps:
- Medications, including antidepressants
- Cognitive behavior therapy, which focuses on shifting patterns of thinking, as well as lifestyle habits
- Hormone replacement therapy
22. Menopause and Panic Attacks
In the menopausal and post menopausal years, about 18% of women report experiencing panic attacks within the past 6 months. Some women have their first panic attack during perimenopause, while others report a worsening of preexisting panic disorder. An episode can involve an intense feeling of fear, sweating, shortness of breath, and may even be mistaken for a heart attack. It may last a matter of seconds or much longer, and can be triggered by a specific event or seem to come out of the blue, for no apparent reason.
The estrogen and progesterone changes that can lead to anxiety, described above, also contribute to panic attacks. But just like other psychological symptoms that come with menopause, panic disorder can be managed with the right support and help.
What helps:
- Regular exercise and paced breathing practice
- Cognitive behavior therapy
- Medications such as anti-anxiety and antidepressants
There are even more surprising symptoms of menopause, which actually shouldn’t be surprising given the wide ranging effects of hormone transition throughout the body. The list grows as research continues and clinicians report what they’re seeing in practice. Moreover, every woman’s experience is unique, so talk to your Midi clinician, or another doctor supporting you in midlife, about anything you’re feeling. As we say often at Midi: You know your body. We know the science. Let’s work together to help you feel your best.
The Takeaway
- As women reach midlife and approach menopause, estrogen levels naturally decline.
- Estrogen depletion affects pretty much everything—your hair, teeth, skin, nails, as well as brain function—so surprising symptoms may crop up in all areas of your health.
- Whatever arises for you, there’s no need to simply power through it. You can make a difference in your health through lifestyle changes and wellness therapies (for example, acupuncture or cognitive behavior therapy), as well as taking supplements, botanicals, and/or prescription medications.
- Hormone replacement therapy (HRT), targeted to your individual history and needs, is the most effective treatment available and can alleviate many of these symptoms. HRT isn’t for every woman, however, and expert prescribing is a must, so seek out a Midi clinician or other hormone specialist for personalized guidance.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.
 Redeat Gebeyehu
Redeat Gebeyehu





