If your doctor won’t prescribe hormone replacement therapy, you’re not alone. Here, at Midi Health, we hear from many women who have faced barriers to receiving the right care for their perimenopause and menopause symptoms. This can be frustrating when you know what you’re feeling—and what you need to feel better. The good news: You’re not stuck. Working with a healthcare professional, like a Midi clinician, who is specifically trained in menopause can make a big difference in the care you receive. Still, there are ways you can bridge the gap with your current provider. Read on to find out how to have a productive conversation.
When menopause symptoms start to pop up, it can feel a little more like whack-a-mole than a clear cut problem and solution. The night sweats started, but maybe it was because it was summer. Or maybe it was because you gained weight. Oh, right, you gained weight. But that might have been because of your most recent, carbs-don’t-count vacation. You’ve been having insomnia, but that might be because you’ve been stressed….and so on and so on.
It’s hard to connect the dots (especially if you’re suffering from yet another symptom—brain fog!), but when you finally do, you might be ready for some symptom relief in the form of hormone replacement therapy, like, yesterday. Your doctor, though, might not be as ready as you are. (Hormone replacement therapy, or HRT, is also referred to as menopausal hormone therapy or MHT. We’ll use HRT throughout this article.)
“A lot of providers are reluctant to talk about menopause because they’re uncomfortable with it,” says Midi clinician Sonya Carothers, PhD, a family nurse practitioner and Certified Practitioner from the Menopause Society. “Providers know about hormone replacement therapy, but they’re still hesitant to prescribe it.” This can be for a variety of reasons, from lack of training to outdated research.
Use this helpful guide to plan your conversation with your doctor so you’re ready to get what you need, which may ultimately include expanding your care team to add a Midi clinician (who can work with your other doctors).
Understanding the Importance of Hormone Replacement Therapy
In the years leading up to your final period—known collectively as perimenopause—your body undergoes a slew of physiologic changes that can result in everything from hot flashes and vaginal irritation to low bone mass and a shorter emotional fuse.
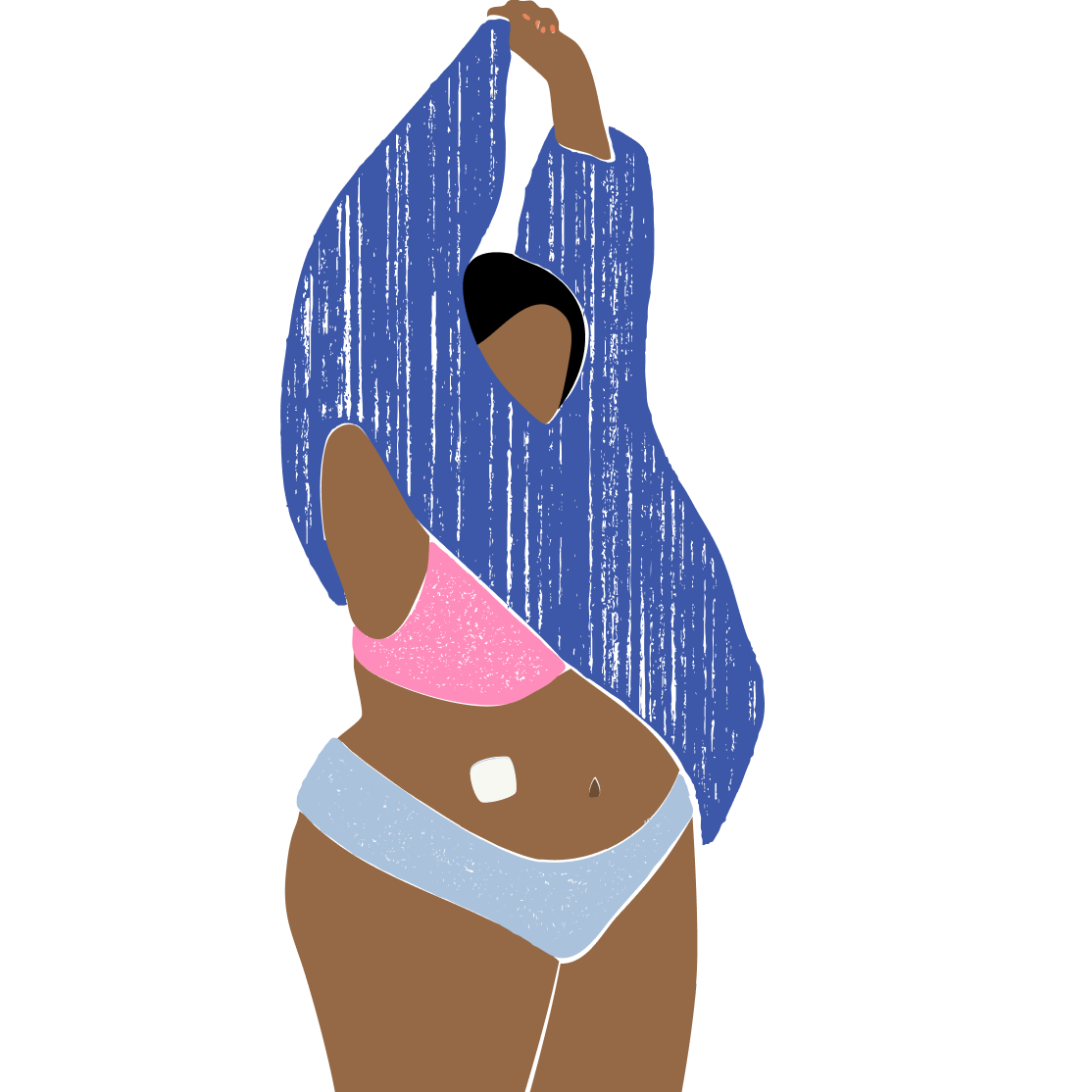
With hormone replacement therapy, a combination of estrogen and progesterone (for women who still have their uterus) or estrogen alone (for women who’ve had their uterus removed) is used to help ease some of the more difficult symptoms.
Available in many forms, including pills, patches, topical creams and gels, and vaginal rings, HRT works by releasing hormones into the bloodstream or vaginal tissues. That said, the acronym “HRT” is somewhat of a misnomer—you’re not replacing these hormones as much as supplementing them as they naturally decline. “The most common formulations do boost estrogen and progesterone, but the amount does not come close to fully replacing our prior levels,” says Midi’s Chief Medical Officer Kathleen Jordan, MD. But HRT is so powerful that adding back just a tiny percentage of the hormones your body made during your peak reproductive years “is all that is needed to gain so many benefits,” she adds.
In the past 20+ years, research has shown women who start HRT within 10 years of their last period not only enjoy significant relief from menopausal symptoms, but their future risk of heart disease, bone loss, and diabetes improves, too.

Common concerns about hormone replacement therapy
Of course you trust your healthcare team to make the best decisions for you. But sometimes, they think not prescribing hormone replacement therapy is the right decision, due to outdated research.
“The most common reason doctors are hesitant to prescribe HRT is that in 2002, the Women’s Health Initiative released a study citing a link between HRT and breast cancer,” says Dr. Carothers. However modern forms of HRT, such as transdermal estrogen and bioidentical progesterone, have not shown to increase breast cancer risk in the way it was first concluded from the WHI. Other providers fear the risk of blood clots in estrogen therapy, but transdermal estrogens have been found to pose a much lower risk than estrogen in pill form.
It’s been frustratingly difficult to shake the misconception that HRT is unsafe, but, at Midi, we support its use and prescribe it responsibly. That means partnering with you on a personalized Care Plan based on your unique symptoms, risk factors, and approach to wellbeing.
When should I start hormone replacement therapy?
Hormone replacement therapy (HRT) is the most effective treatment for relieving hot flashes, night sweats, and vaginal dryness and preventing osteoporosis. But Midi patients often ask us if it’s too early—or late—to start treatment. Every Care Plan is personalized for your symptoms and health history, but these general guidelines often hold true:
- The earlier, the better. It’s best to start HRT within 10 years of your last period, since you’ll get the added benefit of a lowered risk of heart disease and bone loss. But you don’t need to wait for your period to stop. If you’re having symptoms, you can begin HRT—even if you’re in perimenopause.
- Missed that 10-year window? If menopause symptoms are messing with your quality of life, it’s still worth considering HRT. A Midi clinician can talk you through the risks and benefits. (Know that you may miss out on the heart-bolstering benefits if you start outside the 10-year window.)
- Localized vaginal estrogen is fine anytime. Dealing with dryness, painful sex, urinary problems? Vaginal estrogen creams, rings, or suppositories are incredibly effective and safe for nearly all patients at any time.
True Stories Of Transformation
Potential Reasons Why Your Doctor Is Against Prescribing HRT
We like to imagine that our doctors are well versed in, well, everything. But the truth can look a bit different than that. Reasons your doctor may be against HRT:
- They lack proper training. “Menopause isn’t really taught in medical school or residency,” says Dr. Carothers. Because of this lack of education, some doctors might find themselves hesitant to prescribe hormone replacement therapy.
- Concerns about your medical history. Your doctor will also be considering your medical history and any preexisting conditions like breast cancer, blood clots, or cardiovascular disease, and they might be weighing those against the benefits of HRT.
- Regulations. A doctor’s healthcare institution might have policies that make prescribing HRT more arduous.

Key Benefits of HRT
The biggest benefit of hormone replacement therapy is that you finally can start feeling more like you again. But keeping your estrogen levels higher can have benefits that extend way longer than just perimenopause.
- Stronger bones: HRT significantly reduces the risk of fractures and is effective in preventing osteoporosis in postmenopausal women.
- Healthier heart: Some research has shown that starting HRT ten years before menopause can reduce your risk of heart disease.
- Sharper brain function: We all want to stay sharp as we age and protect the brain against cognitive decline that can start in the menopausal years. While HRT has not yet been shown to treat brain fog or cognitive changes, for a subset of high risk women, HRT may be protective of their cognitive function based on early research.
- Improved vaginal health: Local estrogen therapy is highly effective in treating vaginal dryness, atrophy, and urinary symptoms—all things that can make daily life and sex more uncomfortable.
What's Best For You?
While menopause looks different for everyone, you’ll start to recognize some of the most prominent symptoms over time—and the ones that are the most prevalent for you.
“It’s easy to dismiss your first hot flash,” says Dr. Carothers. “Another one might not happen for another three to four years. But having the symptoms top of mind can help you be prepared to bring them up with your doctor.” Dr. Carothers says the conversation with your doctor could also come when you’re in your 40s, or if you’re ready to talk about going off hormonal birth control because of a tubal ligation or another procedure.
“A lot of times birth control will mask the symptoms of perimenopause, so it can be a good opportunity to discuss HRT when you are coming off the pill,” says Dr. Carothers. In conversation, make sure that you focus not only on your symptoms but on your quality of life and your individual risk. You can also ask if there are non-hormonal treatments that your doctor recommends, like supplements.
How to Discuss HRT with Your Doctor
You know how when something is top of mind for you, suddenly you see it everywhere? That kind of recency bias happens with everything—including conversations about menopause. If your friends and family are in a similar life stage with you, they might easily attribute any of your symptoms to things they’re going through in their own menopause journey, making the answer to your problems feel woefully obvious and easy to fix. But your doctor sees patients all day, of all ages, with all sorts of various problems, and only has a short appointment to get to the bottom of each one. That’s why it helps to be very prepared for your conversation.
Whatever your symptoms, Dr. Carothers recommends logging them, when they started—to the best of your memory—and how often you’re experiencing them so that you can bring this info with you to your doctor’s appointment. Be sure to highlight how your symptoms are affecting your day-to-day life. You can include things like, "My brain fog is affecting my ability to perform at my job" or "Vaginal dryness has prevented me from being intimate with my partner." The more specific you can be, the better.
Dr. Carothers also says that it’s helpful to do some research on types of hormone replacement therapy and how they might work for you. HRT comes in many different forms, and finding the right one for your lifestyle is a conversation you can have with your doctor. Here’s a helpful guide for having a conversation with your doctor.
- Be honest. “Some doctors might not connect symptoms like recurrent UTIs with vaginal dryness from menopause,” says Dr. Carothers. Connecting the dots for them might help lead them through the conversation.
- Focus on timing. When talking about your symptoms, it can be helpful to frame things in the lens of “When I turned 45….” to add context to this unique period of life. “Menopause is a developmental stage, just like puberty,” says Dr. Carothers. Being clear that symptoms started in the prime of your perimenopausal years can help your doctor identify unique needs that you might not have had before.
- Be direct, and ask for what you want. “This is about you getting relief for your symptoms,” says Dr. Carothers. “Don’t be afraid to say, ‘I’m 45 years old now, and I’m finding my X, Y, and Z symptoms very difficult, and I’d like to try hormone replacement therapy. Can you help me navigate this?’”
- Be persistent. If a doctor is hesitant, ask about your specific risk factors, and if there are options that are better for you, like transdermal estrogen if you have a history or are at risk of blood clots. Dr. Carothers also suggests requesting a trial: Ask whether you can do a trial with HRT, and follow up with your results.
- Make a plan. If your doctor isn’t willing to prescribe right away, set a time to follow up two weeks later, even if they suggest a six month follow-up. “There’s no need to struggle with your symptoms because your doctor isn’t prepared,” says Dr. Carothers. Follow up sooner to get relief faster. You can also ask if there’s another specialist that they can refer you to who might be able to help or seek out support on your own, like booking a visit with a Midi clinician.
- Ask questions. If you’re being met with resistance, make sure to ask why and push your doctor to help you to find a solution while you’re in the appointment together. Ask questions like: What are the specific reasons for hesitating to prescribe HRT in my case? Can we explore different types and doses of HRT that might be safer for me? How do we monitor my care to make sure I’m safe on HRT? Should I see a menopause specialist for a second opinion?
Bring This Checklist To Your Next Appointment
Doctor’s appointments can go by in a blur. To make sure you get the most out of the conversation—and leave with what you need—focus on your symptoms, medical history, risks, and options.
- Discuss Your Symptoms: Come to the appointment armed with a log of your menopausal symptoms, including info on their intensity and frequency. If you can pinpoint any patterns, share that too.
- Review Your Medical History: Be open and honest about your family medical history, especially a history of cancer and other chronic conditions.
- Ask About Risks and Benefits: Ask how HRT could affect your individual health risks—and how it can improve your quality of life.
- Explore Different HRT Options: Discuss various forms of HRT, such as transdermal vs. oral, bioidentical hormones, and localized treatments. If your most bothersome symptom is vaginal dryness, for example, your treatment can be much more focused. If your vasomotor symptoms are the ones driving you crazy, you might benefit from systemic HRT.
- Talk About Monitoring and Follow-up: Ask about regular check-ups and how your health will be monitored while using HRT.
- Ask For Non-Hormonal Alternatives: If HRT isn’t recommended for you, ask your doctor what your non-hormonal treatment options might be. You should still leave your appointment with hope that you can get relief.
Key Takeaways
- Don’t shy away from tough conversations with your doctor if they don’t offer you HRT for menopause-related symptoms.
- You know your body best and are your best advocate, so come prepared with your symptom tracker along with questions to get the most out of the conversation.
- Educating yourself about hormone replacement therapy, and guiding the conversation with your doctor about hormone replacement therapy can help you get the relief you need.
- While you may want your existing doctor to remain part of your care, seeking out help from a menopause specialist, like a Midi clinician, can help you feel heard—and feel better.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including vaginal dryness and irritation, brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.