Menopause brings a bunch of uncomfortable (and oftentimes intimate) symptoms. Vaginal dryness is one of the most common. Declines in estrogen during midlife cause changes to vaginal tissues that lead to not only dryness down there, but also irritation and pain during sex. But you don't have to suffer in silence. A well-rounded treatment plan that incorporates healthy lifestyle factors, natural solutions, over-the-counter products, and possible prescription treatments can bring back moisture and elasticity that help you feel good in the bedroom and as you go about your daily life.
Let’s cut right to it: The hormonal changes that come with the menopausal transition do a number on your vagina—with vaginal dryness being one of the most common and uncomfortable symptoms of declining estrogen levels.
That said, here’s the good news: Vaginal dryness is one of the most treatable symptoms of menopause. You don’t have to just deal with it—solutions exist, ranging from medical therapies to lifestyle and natural remedies. Read on to find out more about why perimenopause and menopause changes vaginal lubrication and what you can do to feel better.
What Is Vaginal Dryness?
If your privates are parched, you’ll no doubt feel it. Vaginal dryness refers to vaginal tissues that are not well lubricated. This occurs when the vagina produces less of the fluid that keeps these tissues moist. This happens when estrogen—the main hormone responsible for maintaining vaginal blood flow and lubrication, and keeping your vaginal walls elastic—starts fluctuating and declining during perimenopause and menopause (as you reach the end of your reproductive years). As levels drop, tissue in both the vagina and the vulva become thinner, dryer, weaker, and prone to irritation.
Less natural lubrication is associated with several factors:
- Decreased vaginal blood flow
- Thinning of vaginal tissues
- Changes to the microbiome
- Inflammation
One thing to note: You may hear vaginal dryness referred to by a few different names, including vaginal atrophy, vulvovaginal atrophy, atrophic vaginitis, and genitourinary syndrome of menopause (GSM). Midi clinicians use GSM when discussing vaginal dryness and associated symptoms.
Symptoms of Vaginal Dryness
Being dry down there is a big deal because it impacts your comfort and life in so many ways, including:
- Abnormal vaginal discharge that is thin and white. (This type of discharge does not have a foul odor. That said, sometimes abnormal discharge can be a sign of infection, so it’s a good idea to contact a healthcare professional, like a Midi clinician.)
- Decreased sexual satisfaction
- Low libido
- Pain during intercourse
- Vaginal burning
- Vaginal irritation
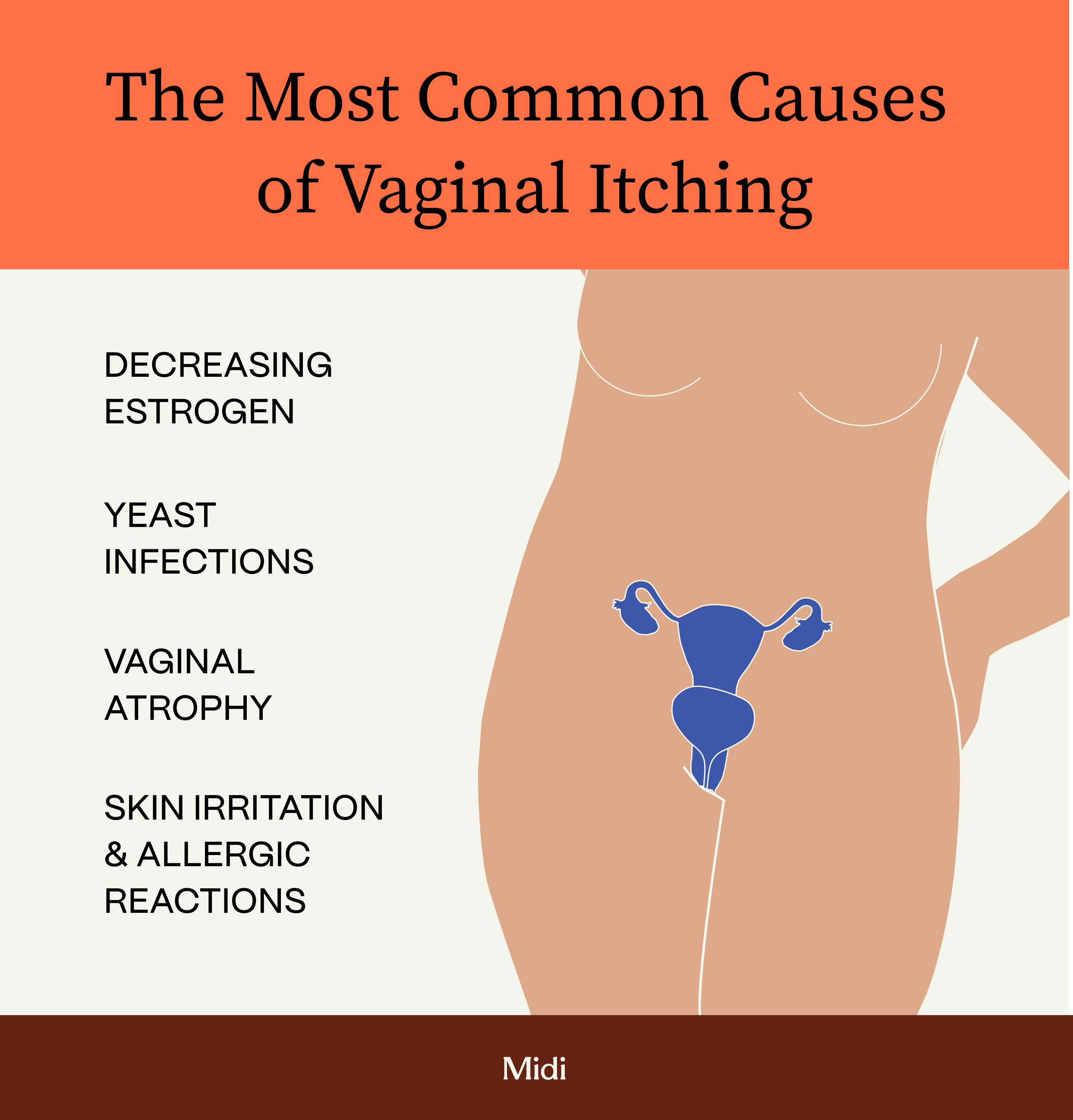
- Vaginal itching
These vaginal symptoms can of course be felt during sex, but they’re also common at other times, like when you’re running errands, working, taking a Pilates class, and so on. According to one report, about 60% of women say vaginal dryness not only affects their enjoyment of sex, but that it also interferes with their sleep, temperament, and–yes–enjoyment of life. Don’t discount how you’re feeling as not a big deal. Midi clinicians have seen and heard it all and, most importantly, they can help.
Common Causes of Vaginal Dryness
As we’ve covered, declining estrogen levels during perimenopause and menopause can be to blame for vaginal dryness. Estrogen is the hormone that keeps vaginal and vulvar tissues thick, elastic, and moist.
There’s evidence that the likelihood of having vaginal dryness increases as you march through the menopausal transition, according to research in the journal Menopause. About one in five women ages 42 to 53 years old reported vaginal dryness, a rate that increased with time. By the time these women were 57 to 69 years old, one in three had reported dealing with vaginal dryness.
You can also have a decline in estrogen caused by the surgical removal of the ovaries (known as surgical menopause), cancer treatment consisting of chemotherapy or radiation to your pelvis, autoimmune conditions like Sjögren’s syndrome, frequent breastfeeding, or certain medications, such as birth control injections, cold and allergy meds, and some antidepressants.
There are also lifestyle factors that may be at play, and it’s worth thinking about if any of these are currently in your routine:
- Using harsh soaps, lotions, or douching, which cause irritation, dryness, and impact your vaginal microbiome.
- Spending time in swimming pools or hot tubs (their chemicals can also affect your vagina’s microbiome)
- Smoking
- Tampon use (some women find that these feel drying to the vagina)
How Vaginal Dryness Is Diagnosed
Don’t hesitate to bring up vaginal dryness to a healthcare professional, like a Midi clinician. But we get that it may not be easy. After all, discussing this topic can be as uncomfortable as your vagina feels right now. Still, being open and honest about everything you're feeling is the best first step in getting help. (Only about 50% of women speak up about this problem, finds earlier research.)
Speaking with a trained menopause specialist can help as they have experience diagnosing and treating vaginal dryness. “There is a lack of medical training on female sexuality and age-related concerns, so it is important that women find a provider that’s open to discussing these concerns, is knowledgeable, makes a woman feel heard, and validates her concerns,” says Midi’s Chief Clinical Officer Mindy Goldman, MD, who’s been a practicing OB/GYN at the University of California, San Francisco (UCSF) for almost 30 years.
During an appointment, expect to talk about your medical history and the symptoms you’re experiencing. Don’t forget to include how vaginal dryness is impacting your life, such as your sleep, daytime comfort, or sexual satisfaction. You may be referred for a pelvic exam to assess the health of your vagina, as well as lab tests, if necessary, to rule out underlying health conditions.
Health Impacts of Untreated Vaginal Dryness
If you're tempted to downplay your vaginal dryness as "not a big deal," don't. During menopause, vaginal dryness may be part of GSM (refresher: genitourinary syndrome of menopause). GSM is a condition that encompasses vaginal and sexual symptoms, as well as urinary symptoms like urgency, incontinence, and recurrent UTIs. GSM is a chronic, progressive condition, meaning it’s one that gets worse without treatment and doesn’t just “go away” on its own.
When vaginal dryness (and GSM) goes unchecked, it can affect so many areas of your life, including:
- Your sex life and sexual satisfaction
- Your relationship satisfaction with a partner
- Long-term sleep problems, if symptoms are causing discomfort at night. (And there are a whole lot of issues that come with poor sleep overtime.)
- Recurrent vaginal infections and/or urinary tract infections
- Decreased quality of life
Treatments for Vaginal Dryness
To get your vagina’s moisture back online, the goal is twofold:
- Address symptoms to improve comfort in life and during sex.
- Treat the underlying cause to help vaginal tissues naturally produce more moisture on their own.
And to get that done, you have some very hepful, science-backed options:
Over-the-Counter Solutions for Vaginal Dryness
Vaginal moisturizers and lubricants are your BFFs right now. Both sound the same, but they have different uses.
- A vaginal moisturizer is something you apply a few times per week, and it works by improving moisture in vaginal cells so that you’re naturally more hydrated. Midi clinicians recommend the vaginal moisturizing products by the brands Good Clean Love and Revaree by Bonafide. You can liken it to a moisturizer you apply to the dry skin on your face, in that regular use keeps you well-hydrated. (Just never apply facial lotions to the skin or tissues down there—it’s a recipe for irritation and pH imbalance. Vaginal moisturizers are specifically used for the vagina.)
- A vaginal lubricant, on the other hand, is a product that you use during sexual activity. These products make penetration more comfortable and a whole lot more enjoyable. If you’re using condoms, you’ll want to ensure that the lubricant you’re using is also condom compatible. (That includes silicone- and water-based lubes, but often not oil-based ones.)
No matter what OTC product you’re using, make sure that it’s fragrance-free (and, if a lubricant, also free of colors and flavorings) to protect the health of your vagina.
Prescription Treatments for Vaginal Dryness
Menopause is considered a time of “estrogen deficiency.” Since this loss of estrogen is a primary cause of many cases of vaginal dryness, one gold-standard treatment is local, low-dose (non-systemic) hormone replacement therapy (HRT). Vaginal estrogen cream—aka “skincare for down there”—is inserted with an applicator for intravaginal use. You can also apply externally to the vulva to restore moisture to parched vaginal tissues. There are also prescription vaginal rings (i.e. Estring) and suppositories (like Vagifem). Many women will stay on creams long-term, which keeps vaginal tissues hydrated and happy.
If you have additional symptoms of menopause like hot flashes and night sweats, your clinician may also recommend systemic HRT. This type of HRT supplies estrogen and/or progesterone (if you have a uterus) to the body, and it is available in a variety of forms, including pill, patch, and vaginal ring. Using HRT can improve the health of the tissues that line the vagina and vaginal pH and increase moisture. It’s been found to improve GSM symptoms in three out of four women. Vaginal estrogen cream and systemic HRT can be used together safely.

Vaginal Dryness Natural Remedies
Although the over-the-counter and prescription treatments will be the most impactful on vaginal dryness symptoms, don’t discount the role of healthy lifestyle habits.
Dietary Changes
Several foods provide phytoestrogens to support overall hormonal health–and there is research in JAMA to show that phytoestrogens may help improve vaginal dryness. These are compounds found in some plants that have weak estrogen-like activity and are found in soy (tofu, edamame, soybeans, soy milk), flaxseed, whole grains, and tea.
Exercise
In addition, pelvic floor exercises have also been found to improve down-there blood flow and tissue elasticity in postmenopausal women with GSM. (A pelvic floor therapist can teach you these exercises and develop a customized plan for you to follow.)
Stress management
Lack of lubrication during sex can also be caused by factors like relationship problems and stress. Stress can tank libido (and lubrication along with it) in numerous ways, but it also throws your hormonal health out of whack. Stress management and caring for your mental and emotional health can make a difference. Consider practices like a daily meditation app, connecting with a therapist, meeting with friends, going for daily walks, reading enjoyable books, and reconnecting with your partner.
How to Prevent Vaginal Dryness
All of the things we discussed above also come into play when we’re talking prevention:
- Maintain a balanced diet and stay hydrated by drinking water
- Get adequate sleep
- Care for your sensitive skin down there by using water or a mild soap to wash up. Avoid fragrances.
- Exercise—although it doesn’t directly treat vaginal dryness, it’s a habit that reduces stress, improves sleep, and supports your metabolic health, all of which are linked to sexual health.
- Talking to a healthcare professional, like a Midi clinician, once you experience symptoms of menopause, after undergoing treatments that affect your ovaries, or after a health diagnosis that impacts your estrogen levels. Treating vaginal symptoms early can help you avoid years of discomfort.
- Have sex! Intercourse helps maintain the elasticity of vaginal tissues. (This can also be part of a treatment plan, but you want to make sure that sex feels comfortable first with the above methods like using vaginal moisturizers and/or lubrication.)
When to See a Doctor for Vaginal Dryness
Data shows that genitourinary syndrome of menopause commonly goes underdiagnosed and undertreated. That doesn’t have to be the case for you. If you are experiencing any persistent and bothersome symptoms of vaginal dryness that impacts your daily life, connect with a menopause-educated clinician like one at Midi who will work with you to develop a care plan individualized to your needs, including over-the-counter products, lifestyle coaching, natural remedies and supplements, and prescription treatments, if needed. If you have concerns about underlying health conditions, see a clinician for a thorough exam and possible testing.
The Takeaway
- Vaginal dryness is incredibly common among women during the natural course of the menopausal transition as estrogen levels fluctuate and decline. Estrogen is a group of hormones that keeps vaginal tissue thick, elastic, and lubricated, so as it declines, you may notice more discomfort and irritation.
- Vaginal dryness symptoms include burning, itching, and pain during sex. These symptoms can be part of genitourinary syndrome of menopause (GSM), a condition that includes vaginal and sexual symptoms as well as urinary issues like incontinence, urgency, and recurrent urinary tract infections.
- Treatment for vaginal dryness includes over-the-counter options like vaginal moisturizers and lubricants during sex. In addition, your clinician may recommend hormone replacement therapy (HRT), either or in addition to local vaginal estrogen.
- Lifestyle interventions like eating a healthy diet that includes food sources of phytoestrogens, stress reduction, addressing relationship problems, and more promote both hormonal and overall health and well-being.
- If you are dealing with persistent symptoms of vaginal dryness that’s impacting your daily life, speak with a clinician.
Frequently Asked Questions (FAQs)
How do you fix dryness down there?
The mainstays of treatment for vaginal dryness include vaginal moisturizers, vaginal lubricants, and prescription hormone replacement therapy (HRT). HRT can be systemic (or body-wide) and given as a pill, patch, or vaginal ring or you may be prescribed a local vaginal estrogen cream. A combination of these treatments may be used to give you the moisture boost you need.
What is the best lubricant for female dryness?
Lubricants are used before sex to make your experience more comfortable. Look for one that is free of fragrance, dyes, and flavors. If you are not using condoms, coconut oil can be a natural option.
What is the best way to moisturize your vagina?
Vaginal moisturizers are products designed specifically for this purpose. They're typically used every few days to keep vaginal tissues hydrated long-term, outside of sexual activity.
How can I get wet again after menopause?
Hormone replacement therapy (HRT), available as a local estrogen cream or systemic formula as a pill, patch, or vaginal ring, is a safe and effective way to give your body the estrogen it needs to keep vaginal tissues healthy and…yes…wet. Also keep in mind that mental and emotional factors also play into vaginal lubrication, so assess your relationship health, as well as stress and sleep.
What is the main cause of dryness?
Although there are many causes of vaginal dryness, the most common is declining estrogen during perimenopause and menopause. A decline in estrogen during these years causes vaginal tissue to become thinner, less elastic, and drier.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.
 Jessica Migala
Jessica Migala





