Perimenopause is the transitional phase before menopause, marked by fluctuating hormones, particularly estrogen, which gradually declines —but not in a totally straight line. This stage can cause symptoms such as hot flashes, sleep disturbances, and changes in brain and sexual function. Like puberty, it is a natural hormonal shift, but it can still bring about uncomfortable symptoms. Understanding these changes is key to managing symptoms through treatment and lifestyle adjustments.
What Is Perimenopause?
Perimenopause is so deeply misunderstood—by women, society, everyone—that many of us have no idea we’re even in it when it happens. That needs to change, asap. Because the more you know about the physical transitions your body goes through, the less alone and powerless you feel—and the more likely you are to get support if you need it.
Let’s start with the basic definition: Perimenopause refers to the natural and normal period when your body adjusts to the end of your reproductive years. The name comes from “peri,” a Greek word meaning “around,” which makes sense since it happens in the years before your period stops. It’s also sometimes called the menopausal transition, and we use both terms at Midi.
Menopause, on the other hand, isn’t a stage, but rather a moment: You reach it exactly 12 consecutive months after your last menstrual period. That point in time marks the definite end of your fertility. The average age of menopause is 51, but it may come years later, or earlier.
While menopause is the same for all women in at least a few respects (no more birth control needed, no more periods, tampons, cramps, wrecked underwear), perimenopause is as unique as your individual body. How it feels, when it starts, and how long it lasts varies enormously from one woman to the next.
On average, perimenopause begins in your mid-40s, but it may kick off as early as your 30s or as late as your 50s. Once it starts, it usually lasts around 4 years, but for some perimenopause stretches out up to 10 years. For others, it only lasts a few months. And the variety of symptoms that come along with perimenopause gets a bit mind-boggling, mainly because of the body-wide influence of the hormone estrogen.
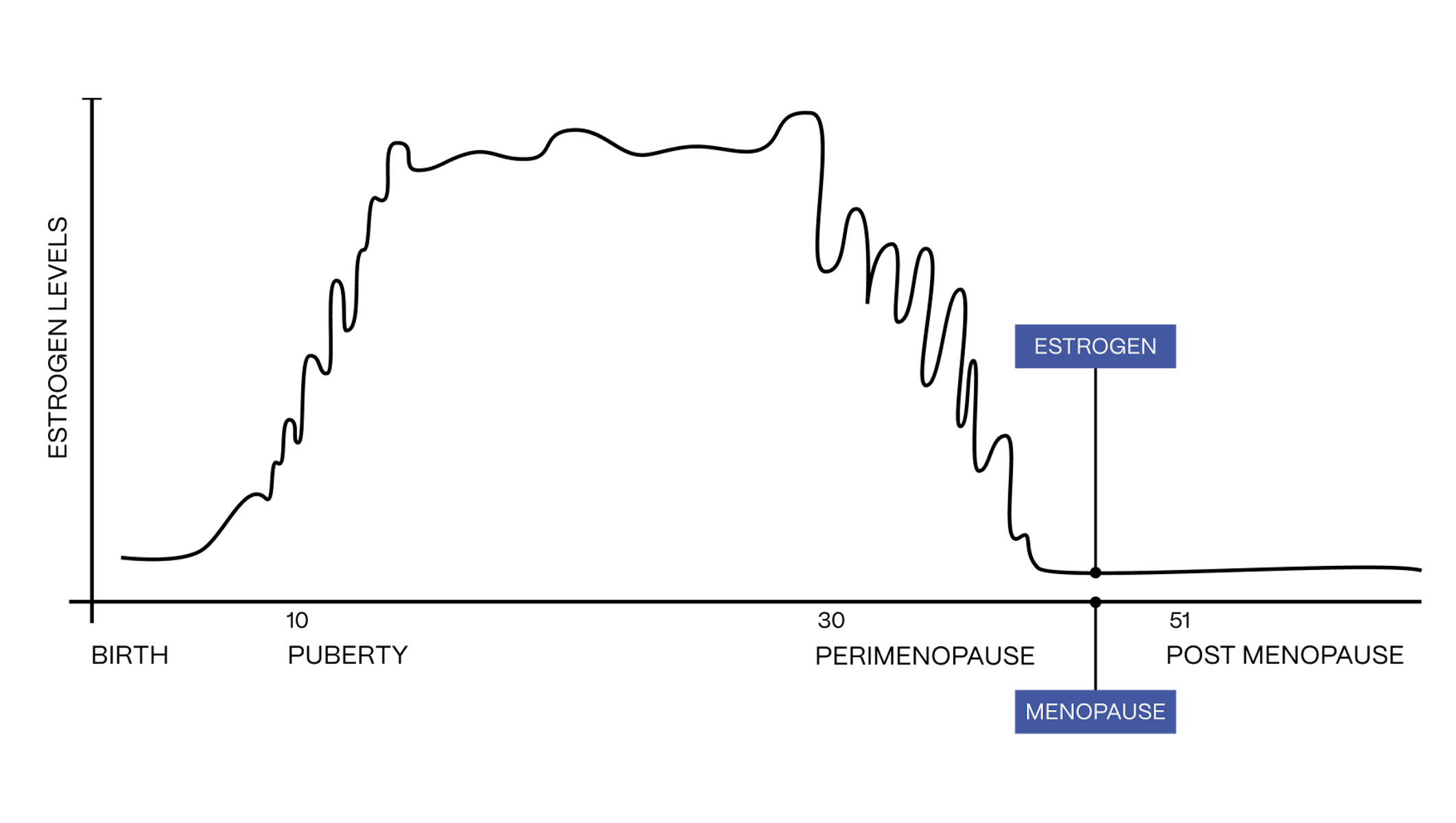
Perimenopause and Hormones
Your ovaries are the main producers of estrogen, which is your primary female sex hormone, influencing nearly every organ and system in your body. The ovaries churn out roughly the same amount of estrogen throughout your fertile years, but during perimenopause, as they gradually wind down their reproductive work, they produce less and less. Don’t picture a steady, predictable decline, though. Estrogen generally trends downward, but fluctuates dramatically along the way, rising and falling unevenly, sometimes dropping very low, other times spiking higher than normal. Eventually, in the later stages of perimenopause, estrogen production sinks so low that your ovaries no longer release eggs. At this point, your monthly periods wrap up, and your ovaries are officially in retirement.
Considering that your ovaries have been producing a steady supply of estrogen pretty much since adolescence, the body is in for a surprise when it begins to roller coaster. Menstrual cycles become unpredictable, and you may experience physical and emotional symptoms. Systems that relied on estrogen may struggle to adjust: For example, research shows that estrogen plays a crucial role in preserving your bone strength and density, so its decrease may lead to bone loss and eventually, osteoporosis. There are several other conditions associated with estrogen depletion and it’s important to look out for them, and seek out the right treatment if necessary.
Am I in Perimenopause?
You can think of perimenopause as your body going through estrogen withdrawal. For some, the experience may feel like a walk in the park, but for others, it’s intense, both physically and emotionally.
The first perimenopause sign is often an erratic menstrual cycle: For most women, studies find, cycles become more and more unpredictable. The stretch between periods can be longer one month, shorter the next, and flow can be heavier this time around, then suddenly lighter. Your period may go missing entirely for months on end, then come roaring back.
Meantime, about 75% of women also experience vasomotor symptoms—hot flashes, night sweats and palpitations—during the menopause transition.
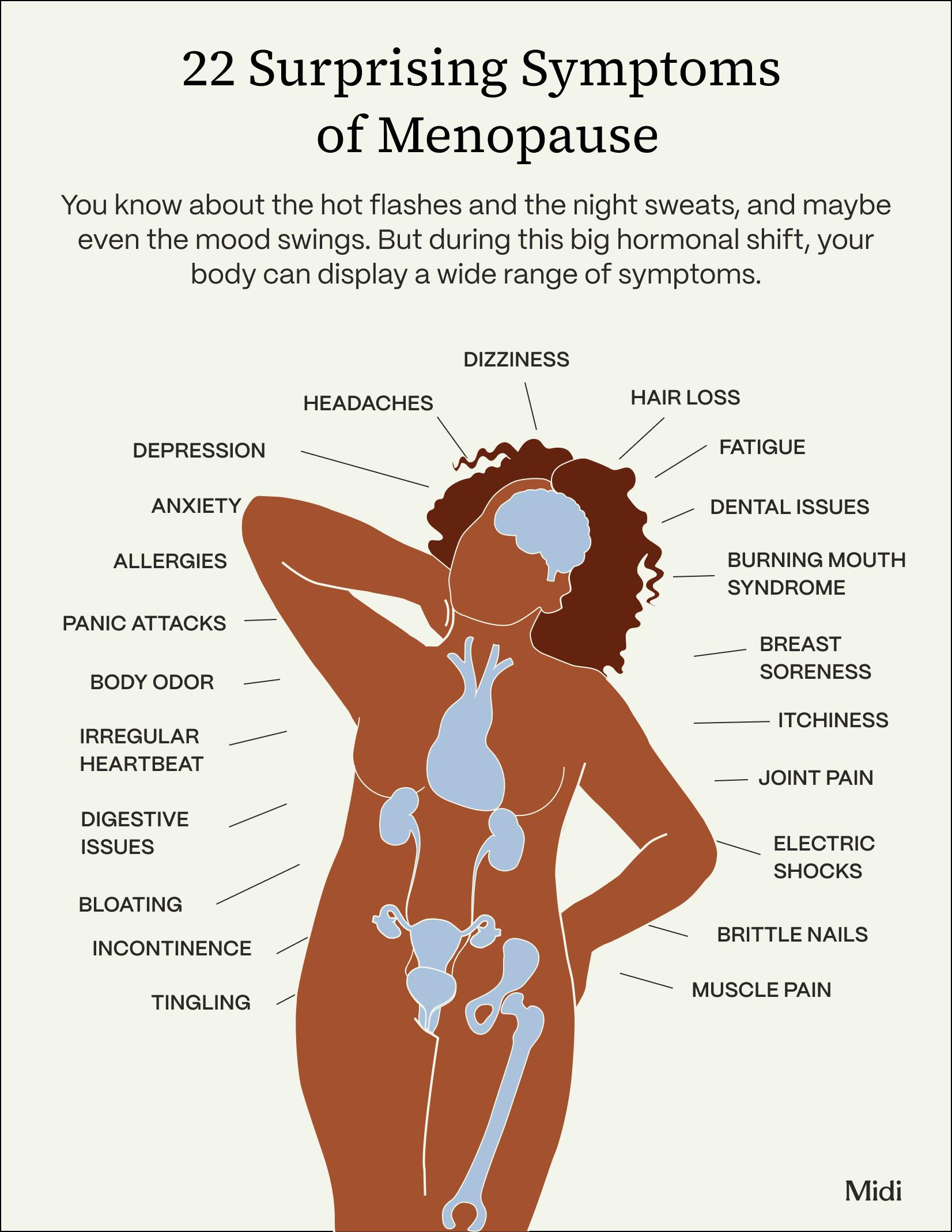
There are a range of other common symptoms which can truly affect you from head to toe including mood swings, difficulty sleeping, brain fog and memory problems, heart palpitations, dental issues —some of which may seem unrelated to hormones, but, yes, these and other surprising symptoms can also be part of the menopausal package for some women.
Perimenopause vs. Puberty
Many experts talk about perimenopause as puberty in reverse, because these two body stages share plenty of common ground. Looking at the graph below, you can see how the estrogen roller coaster during puberty and perimenopause mirror each other, chaotically climbing and falling, respectively.
If you think back to how shifting hormones triggered behavioral and body changes during your teen years, it makes sense that perimenopause would do the same. Some common physical and emotional symptoms that might ring a bell from puberty: irritability, weight gain, acne, mood changes and a general malaise, aka the “blahs.” Research has explored the more serious parallels, emphasizing how hormone fluctuations during these two periods can lead to “development of depression and anxiety, metabolic and cardiovascular risks, and autoimmune conditions.”
Here’s the major difference: During puberty, the entire world recognizes what you’re going through, and biology class explains the physiology behind it. Parents give adolescent kids extra leeway, and teens give themselves grace. If their symptoms rage out of control, the medical establishment stands ready to help them. In perimenopause, though, most women are grinding through a high-pressure life stage, managing work and family demands, meeting sky-high expectations. People lean on you, rather than offering support. Even worse, doctors may tell you that they can’t do much to help—you’ll just have to tough it out.
How is Perimenopause Diagnosed
To compound the perimenopause problem, many women struggle to pinpoint their symptoms, and have no idea they’re connected to hormonal change. For example, fatigue, a common menopausal symptom, can easily be associated with a busy life and total lack of me-time. It can be helped with treatment, but because they’re unsure what they’re experiencing, most women don’t seek any. In fact, according to a 2021 survey, 73 percent of women aged 40 to 65 were not currently treating their menopause symptoms.
The big question then is, how do you know when you become perimenopausal? Unfortunately, there is no test that can predict in advance when you will start the transition or even fully confirm that you’re in the midst of it. What your physician can do is consider your age, the age at which your mother or sister entered menopause, your health history, all the symptoms you might be experiencing, and order a blood test to measure hormone levels. Remember, though, that your hormones are going up and down a lot during this stage, so a single blood test can be misleading. However, running several tests at different times might provide a clearer picture.
Perimenopause Treatments
So perimenopause can be unpredictable, painful, and mysterious, but the most important thing to know is that it’s treatable. Below we cover the major effective solutions, but keep in mind that some of the symptoms you might experience could be associated with other serious conditions, and need to be discussed with a clinician trained in women’s midlife health.
Medical Interventions
Hormone replacement therapy, sometimes referred to as menopausal hormone therapy or MHT, is a treatment used during perimenopause and menopause to replenish hormones, namely estrogen and progesterone, that naturally decline as your reproductive years wind down. HRT has been shown to be the most effective treatment for things like hot flashes and vaginal dryness.
The name is a bit misleading—you’re not replacing any hormones in your body as much as you’re supplementing them as they decline. HRT is the most effective treatment for managing menopause symptoms that result from the rapidly fluctuating changes in estrogen and progesterone. Unless you’ve had a hysterectomy, clinicians add progesterone or progestin to estrogen. This is necessary because, while estrogen is effective in alleviating symptoms, it can also thicken the uterine lining (which is called endometrial hyperplasia), increasing the risk of uterine cancer.
Adding progesterone to HRT for any patient with a uterus is key because it controls thickening and sends the risk for developing uterine cancer back to baseline. For those without a uterus, certain forms of progesterone may still be recommended to help improve symptoms like sleep issues and night sweats. While not every woman is a candidate for HRT, most can safely take it, according to the Menopause Society, which is the leading organization in understanding and researching the health of mid-life women. Discuss HRT with your doctor or a Midi clinician to get good advice and make the right decision for you, your symptoms, and your approach to health.
Birth control can relieve perimenopause symptoms including menstrual irregularity, heavy menstrual bleeding, menstrual pain, and vasomotor symptoms. And let’s not forget that it prevents pregnancy, which is a real possibility when you’re still getting your period.
Certain non-hormonal prescription medications for perimenopause symptoms can be exceptionally effective. Medications such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs) and low-dose gabapentin are all shown to greatly improve hot flashes. There are also anticholineric medications like oxybutynin, hot flash-specific drugs like fexonlinetant, as well as vaginal creams containing estrogen. Every medication can have their side effects and should be discussed with your doctor or Midi clinician.
Non-Medical Interventions
Lifestyle factors heavily influence the experience of perimenopause and studies have shown carrying extra weight, too much alcohol, and lack of exercise are all associated with more severe symptoms.
- Get enough exercise. Physical activity is extremely helpful in improving insomnia, mood, and musculoskeletal pain, as well as psychological symptoms, including depression and anxiety. The goals to hit, according to the American College of Sports Medicine and American Heart Association recommendations, are moderate physical activity for at least 30 minutes 5 times per week, or intense physical activity of at least 20 minutes 3 times per week. Just moving more throughout your day can help you get those minutes, and keep your metabolism healthy.
- Perform weight-bearing exercises such as hiking, walking, or strength training.
- Eat a diet centered on fruits, vegetables, whole grains, lean proteins, and health fats.
- To help handle hot flashes, dress in layers so you can remove clothing if you begin to sweat.
- Improve your sleep hygiene by powering down devices and screens well before bedtime, keeping your phone charging in a space that's not your bedside, and doing relaxing activities before bedtime.
Wellness therapies have also been shown to make a significant difference in perimenopausal symptoms. For instance, a study published on the Journal of The North American Menopause Society states that cognitive behavioral therapy (CBT) can be used to improve hot flashes, depression, and other menopausal symptoms.
Another example is hypnosis, with research indicating a clinically significant effect on reducing hot flashes, as well as improved sleep quality and sexual function.
Last but not least, botanicals and dietary supplements such as black cohosh, soy, calcium, and vitamin E may bring relief.
When to See a Doctor for Perimenopause Symptoms
If your symptoms are disrupting your life in any way—causing you to call out of work, preventing regular exercise, or otherwise forcing you to change your routine to accommodate the pain— then it’s time to seek out support from a healthcare provider. If the root cause of your pain is menopausal hormonal fluctuations, with guidance from a specialist, you can find ways to ease these and other hormonal symptoms.
When meeting with a menopause specialist or gynecologist to discuss your cramps, expect an in-depth discussion of your medical history and typical menstrual cycle. Depending on your symptoms and history, your healthcare provider may order some diagnostic tests such as a pelvic exam, blood test, or an ultrasound. These tests help determine (or rule out) the potential causes of your cramps and guide your treatment.
Midi Patients' Perimenopause Stories
The Takeaway
- Perimenopause is the midlife phase leading up to menopause, which is when reproductive years officially end.
- During perimenopause, hormones fluctuate dramatically, particularly estrogen. Levels rise and fall daily and monthly, but estrogen gradually trends downward, just not in a linear way.
- Women in this stage are vulnerable to a variety of symptoms that affect brain function, temperature regulation (leading to hot flashes), sleep, sexual wellbeing, and more.
- Just like puberty, perimenopause is simply a hormonal transition that indicates passage from one stage of reproductive life to another. Symptoms can improve with treatment and lifestyle coaching, but women need to understand what’s going on in their bodies in order to get the right help.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.
 Liz Krieger
Liz Krieger





