- Hormonal birth control can help manage perimenopause symptoms such as menstrual irregularities, hot flashes, and heavy bleeding while also offering protective benefits like reduced cancer risk and bone loss prevention.
- Despite lower fertility in your 40s, pregnancy is still possible, making a birth control plan essential.
- Progesterone-based birth control can complement estrogen hormone replacement therapy for enhanced symptom management. Working with a healthcare provider, like a Midi clinician, can help you determine the best treatment plan for you.
There are a few moments in life when birth control can require a major discussion: when you become sexually active, before and after you’ve had a baby, and now….perimenopause. Yes, you read that right.
You might be thinking that a major benefit of wrapping up your fertile years is that you can worry less about getting pregnant, but it turns out that birth control—in whatever form you choose—should still be a sex-life priority. “Women are still ovulating in perimenopause and pregnancies can still happen right up until periods stop entirely," says Midi’s Chief Medical Officer Dr. Kathleen Jordan, M.D. “Often these pregnancies are unplanned, so it continues to be important to discuss birth control all the way up until full menopause—or at least until the early 50s, whichever comes first.”

Research shows that as we age, our use of birth control decreases, which in turn can result in unintended pregnancy. And though many people have healthy pregnancies well into their 40s, research also shows that pregnancy in your 40s can carry additional risk of miscarriage, complication, and adverse outcomes. Fortunately, studies have found that hormonal birth control methods generally can help with some of the pesky effects of perimenopause, and they can aid in symptom relief. Long story short: hormonal birth control can be yet another tool in your perimenopausal tool belt—and keep you pregnancy-free at the same time.

"At Midi, we hear a lot from women who stop their oral birth control pills in perimenopause for a variety of reasons—they aren't sexually active, they lose their access to care, want to try non-pharmaceutical approaches, or simply because they think they can’t get pregnant when they suddenly begin to encounter menopause symptoms,” says Dr. Jordan. “That’s when a birth control method can actually be incredibly useful and it can be considered, in essence, a form of hormone replacement."
Read on to learn what you need to know about birth control in perimenopause and beyond.
The Hormonal Birth Control and Perimenopause Connection
Perimenopause refers to the period of time when your body adjusts to the hormonal fluctuations that come as you wind down your reproductive years. Throughout your menstrual cycle, your body’s hormone levels rise and fall with each cycle, but in perimenopause, estrogen gradually declines. This doesn’t happen in a smooth, orderly way, though. Instead, levels spike and drop like a rollercoaster on their way down.
Perimenopause starts, on average, in your mid-40s, but for some women it can kick off as early as your 30s or as late as your 50s. Typically, it lasts around four years, but for some, perimenopause can be over in just a few months or extend up to a decade. Perimenopause concludes when you haven’t had your period for 12 consecutive months. Once that happens—drumroll, please—you’re in menopause.
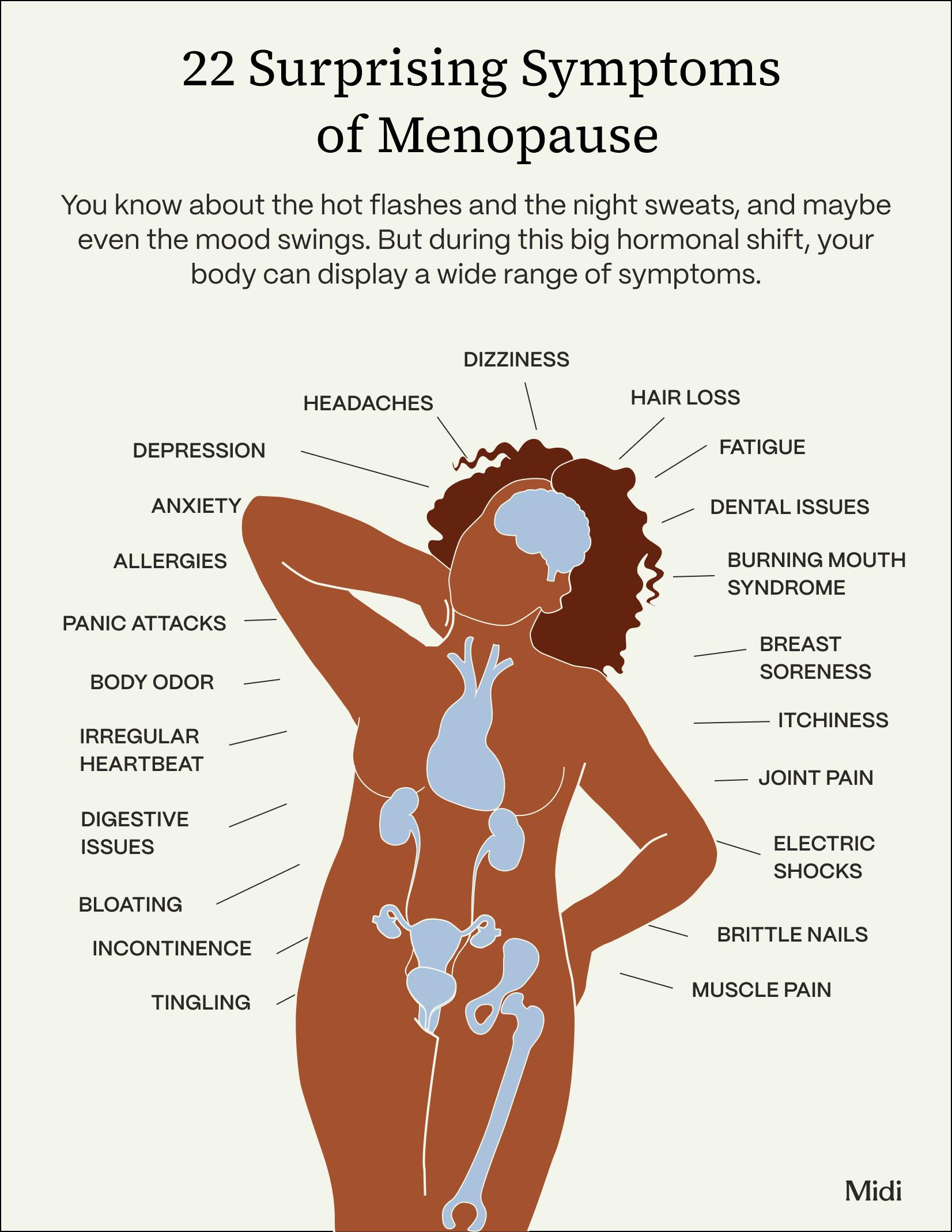
Along with a whole host of symptoms, like night sweats, hot flashes, sleep irregularity, mood changes, joint pain, and brain fog, perimenopause also disrupts your menstrual cycle. Your periods may be shorter, longer, or heavier.
But here’s the thing: While your body is going through all these changes…you can still get pregnant, especially as your cycles become less and less regular and harder to track. That’s where birth control can come in.
“Most birth control pills contain estrogen and progesterone, which are two key hormones that become depleted in perimenopause and menopause,” says Dr. Jordan. “We often treat this hormone depletion with birth control pills in perimenopause, particularly if women are seeking both pregnancy protection and symptom improvement. Taking a combination birth control pill can give women control over their fertility, while also treating their symptoms of hormone depletion that comes with perimenopause.”
Studies have shown that combined hormonal birth control—meaning the types that use estrogen and progesterone to prevent pregnancy (and come in the form of a pill, vaginal ring, or patch)—can relieve many perimenopause symptoms, including:
- Menstrual irregularity
- Heavy menstrual bleeding
- Menstrual pain
- Vasomotor symptoms like hot flashes, heart palpitations, and migraines
Additionally, hormonal birth control can protect against bone loss and reduce the risk of endometrial, colorectal, and ovarian cancer.
Hormone Replacement Therapy (HRT) Vs. Birth Control
Hormone replacement therapy (HRT), sometimes referred to as menopausal hormone therapy or MHT, is commonly suggested as an option for women when it comes to managing the symptoms of perimenopause and menopause in order to replenish hormones, namely estrogen and progesterone, that naturally decline as your reproductive years wind down.
The name is a bit misleading—you’re not replacing any hormones in your body as much as you’re supplementing them as they decline. HRT is available in many forms, including pills, patches, vaginal rings, pellets, topical creams and gels. To protect the uterus (in patients who have one, as opposed to those who’ve undergone a hysterectomy), doctors add progesterone or progestin to estrogen, which reduces any risk of uterine cancer.
HRT does NOT prevent pregnancy, however. And that's often why birth control pills are part of a perimenopause treatment plan for women still ovulating, no matter how irregularly. Let's review the options.
Birth Control Pill
These forms of contraception use estrogen and progesterone with the primary goal of preventing ovulation and making it harder for an egg to implant in your uterus. Birth control pills are taken at the same dose and at the same time every day in a cycle that mimics your menstrual cycle—think 21 days on with 7 days off.
“The dosage of hormones in birth control pills is three to five times higher than the amount in HRT,” notes Dr. Jordan. Many women who are experiencing the first symptoms of perimenopause, especially irregular periods, heavy periods or hot flashes, find that taking hormonal birth control is a win-win—it helps control these frustrating symptoms while also protecting against pregnancy.
Ultimately, the decision to use birth control or any form of hormone therapy should be made in consultation with a healthcare professional, like a Midi clinician, considering your individual health factors and preferences.
And keep in mind: All hormonal birth control comes with risks and side effects. For methods containing estrogen, the side effects typically include:
- Breast tenderness
- Nausea
- Headaches
- Breakthrough bleeding.
There is also an increased risk of deep vein thrombosis (DVT), heart attack, and stroke with estrogen birth control methods, and that risk is higher if you’re over 35, have multiple risk factors like high cholesterol, diabetes, or high blood pressure, have a history of stroke, heart attack, or DVT, or have a history of migraines with aura.
Birth Control Patch
This stick-on method of birth control is an estrogen and progestin combo that’s applied to your shoulder, lower or upper back, or abdomen every month, and removed after three weeks. The patch, however, is not recommended for women over a certain BMI as it can increase your risk of blood clots.
Birth Control Ring
This an estrogen and progestin method that’s inserted into the vagina every month, and removed after three weeks like the patch.

Progesterone Birth Control
Birth control methods that contain progestin but no estrogen won’t necessarily improve hot flashes in perimenopause but they can often significantly reduce menstrual bleeding. They can also make your period irregular or stop it altogether, which some women may prefer. Just know that suppressing your period can make it hard to track your progress toward menopause. One thing to note: Studies have found that progestin methods may exacerbate mood disorders in perimenopausal women who have mental health risk factors.
Hormonal Intrauterine Device (IUD)
This is a progestin method that’s inserted into your uterus by your doctor, and can safely stay put anywhere from three to eight years, so it’s an option you might discuss with your doctor when you’re on the earlier side of perimenopause. It’s also over 99% effective at preventing pregnancy.
Progestin-Only Mini Pill (POP)
This pill is taken daily, and can be an option for women over 40 who have other risk factors that may make them hesitant to use birth control with estrogen.
Progesterone Implant
Inserted by a doctor under the skin, this implant lasts for up to three years. It works by slowly releasing progestin into the bloodstream.
Progesterone Shot
This form of birth control is an injection you receive every three months. The shot has been found to decrease bone density while people take it, so talk to your doctor if you have risk factors for osteoporosis like smoking, previous fractures, steroid use, or a family history.
When HRT and Birth Control Might Be Combined
HRT and birth control can be combined when your birth control method doesn't include estrogen. If you are on a progestin-only birth control, your doctor may suggest adding estradiol, like an estrogen patch, to help control your perimenopause or menopause-related symptoms. The progestin-only birth control will protect your uterus, mitigating cancer risk. If you are on a combination birth control (estrogen & progesterone) this combination will generally control symptoms related to perimenopause/menopause, so HRT may not be warranted to supplement estrogen levels.
Other Birth Control Options for Perimenopause
While hormonal birth control options offer the benefit of menopause symptom relief, there are non-hormonal birth control methods that can prevent pregnancy, like copper IUDs. Barrier methods like condoms, diaphragms, cervical caps, and sponges also work to prevent sperm from reaching eggs, and tubal ligation or bilateral salpingectomy—where your fallopian tubes are removed or cut so eggs don’t travel to your uterus—is a permanent form of birth control. Condoms are the only protection against sexually transmitted infections, or STIs.
Research shows that natural family planning—or tracking your menstrual cycles and avoiding intercourse on days near ovulation—is only about 75% effective at preventing pregnancy during peak fertility years. As cycles get less and less regular in perimenopause, it can be even harder to rely on natural family planning to prevent pregnancy.
Stopping Birth Control in Perimenopause
When to stop birth control is a question to discuss with your clinician, weighing your risk factors, sexual activity, perimenopause symptoms, and HRT plan. Studies have shown that unless you’re high risk, you can safely take combined oral contraception pills until age 55. “Typically once you reach your early 50s or full menopause, we transition from oral contraceptive pills to more traditional estrogen and progesterone therapies,” says Dr. Jordan. “Some women in perimenopause may choose to use birth control in perimenopause purely for symptom management as the dosing of hormones is higher and designed to control ovulation, so it can be helpful if you’re having cyclical symptoms or period irregularities.” You might want to move on to HRT after stopping birth control for symptom relief as well as for the long-term health benefits.
When talking to your healthcare professional, make sure to cover all your options for both your family planning needs as well as perimenopause symptom relief. For many women, a combination of strategies, which may include birth control can help.
Frequently Asked Questions (FAQs)
Can birth control pills help with perimenopause?
Yes, birth control can relieve perimenopause symptoms including menstrual irregularity, heavy menstrual bleeding, menstrual pain, and vasomotor symptoms like heart palpitations, hot flashes, and some migraines. Additionally, hormonal birth control can protect against bone loss and reduce the risk of endometrial, colorectal, and ovarian cancer.
Which type of birth control pill is best for perimenopause?
Your provider will look at your risk factors, needs (i.e. is this for contraception preferences or for treating hot flashes and other vasomotor symptoms?) and previous pill use (if applicable) to determine what is right for you.
At what age should you stop taking birth control?
Talk with your doctor about the right time to stop taking birth control. Experts advise that you can discontinue birth control a year after your last period if your last period was after age 50, and two years after your last period if that happened before you turned 50. You can safely stop taking birth control at 55, after which it’s very unlikely to become naturally pregnant.
Do I need birth control after 45? Some form of birth control is vital anytime you’re still getting your period and don’t want to get pregnant. Pregnancy rates in perimenopausal women with no contraception:
- Age 40-44: 10%
- Age 45-49: 2-3%
- Age 50: less than 1%
Even if your cycles are irregular, you can still get pregnant until you officially go 12 consecutive months without a period.
The Takeaway
- Hormonal birth control for perimenopause can help with symptoms like menstrual irregularity, heavy menstrual bleeding, menstrual pain, and vasomotor symptoms like heart palpitations and hot flashes. Additionally, hormonal birth control can protect against bone loss and reduce the risk of endometrial, colorectal, and ovarian cancer.
- While the risk of getting pregnant in your 40s is lower than when you’re younger, it’s still possible, so a plan for hormonal or non-hormonal birth control in perimenopause is essential.
- When using progesterone birth control, adding estrogen hormone therapy via HRT may help mitigate vasomotor or other perimenopausal symptoms.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including vaginal dryness and irritation, brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.
 Brittany Burke
Brittany Burke