Heavy periods after 40 with clots are common during perimenopause, thanks to shifting hormones that can make bleeding heavier and less predictable. One month, you might notice jelly-like blood clots on heavier days. The next month, your period might be longer or shorter than usual.
Most of the time, these changes are normal—frustrating and inconvenient, yes, but normal. Other times, they're a sign you're losing too much blood or that something else is going on. At Midi Health, our clinicians have seen and treated it all. Here, we'll break down what heavy bleeding with clots can mean, what's typical in your 40s, and when it's time to get checked out.
If you're over age 40 and it seems like your periods have suddenly gotten heavier—or you're seeing blood clots that make you do a double take—you're not imagining things. For many women, an irregular period is one of the first signs that perimenopause has arrived.
Estrogen and progesterone, the hormones that usually keep your menstrual cycles humming along, start bouncing around during this transition. So you might notice all kinds of changes, like cycles that are longer or shorter than usual and heavier periods with clots.
While everyone's cycle is different, a heavy period refers to excessive or prolonged bleeding that gets in the way of your daily life. And here's the thing: Shifting hormones aren't the only reason you might have heavy periods after age 40 with clots. Certain conditions like fibroids or polyps and medications like blood thinners could also be behind it.
So, how do you know what's common and what's not? We've got you covered. Read on to find out what a heavy period actually means, why blood clots happen, and when it's time to check in with a healthcare professional. Plus, get tips to track your cycles and manage symptoms while you figure out next steps.
What Counts as a Heavy Period?
A heavy period isn’t just about how much blood you lose. It’s heavy menstrual bleeding (aka menorrhagia) that’s hard to manage or disrupts your daily routine. That might look like changing pads or tampons more often or passing blood clots during your period.
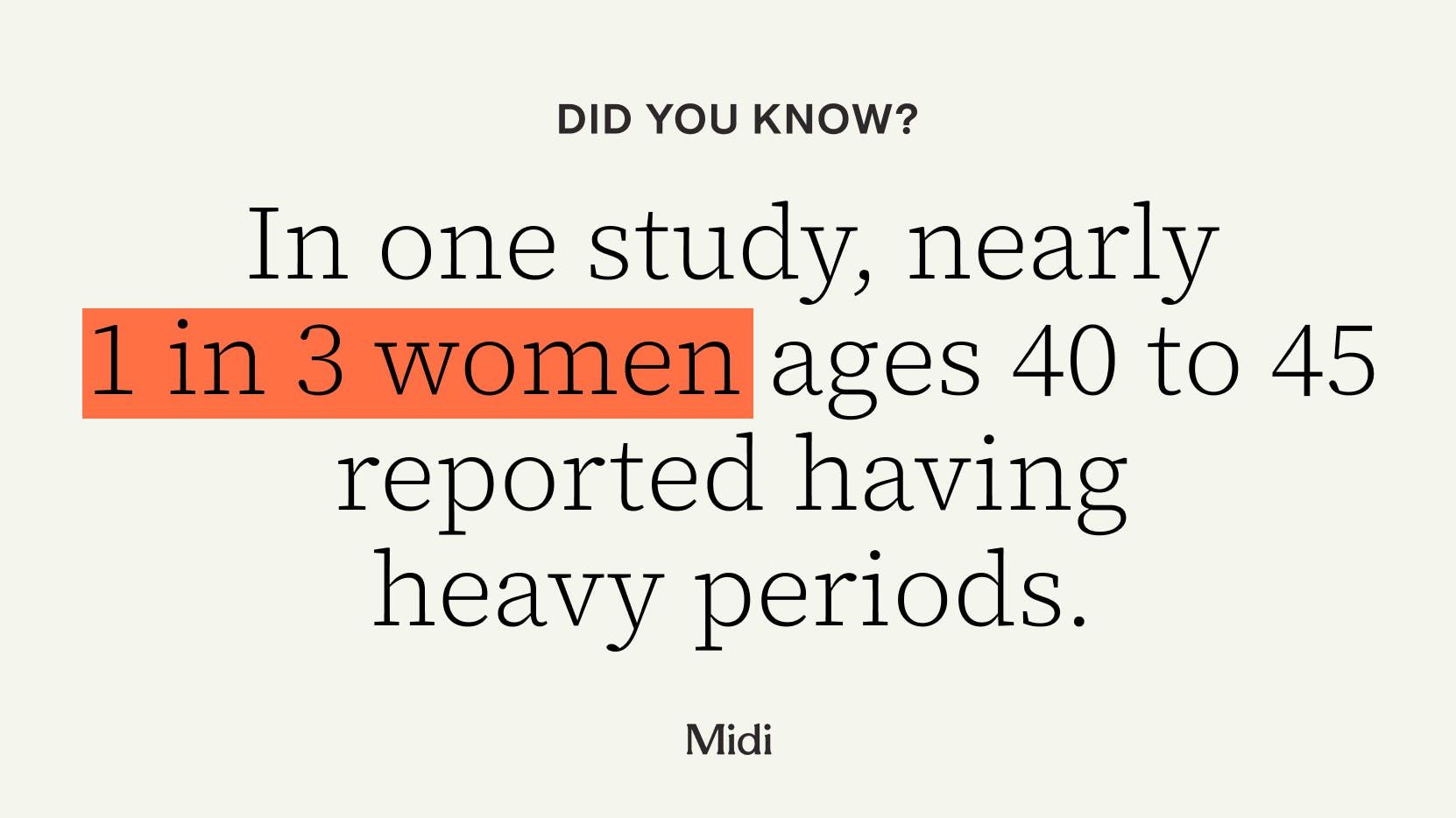
Over time, it can understandably take a toll on your mood, energy, and overall well-being. In one study, nearly 1 in 3 women ages 40 to 45 reported having heavy periods. They were also more likely to report having trouble with work and social activities, as well as just getting through the day.
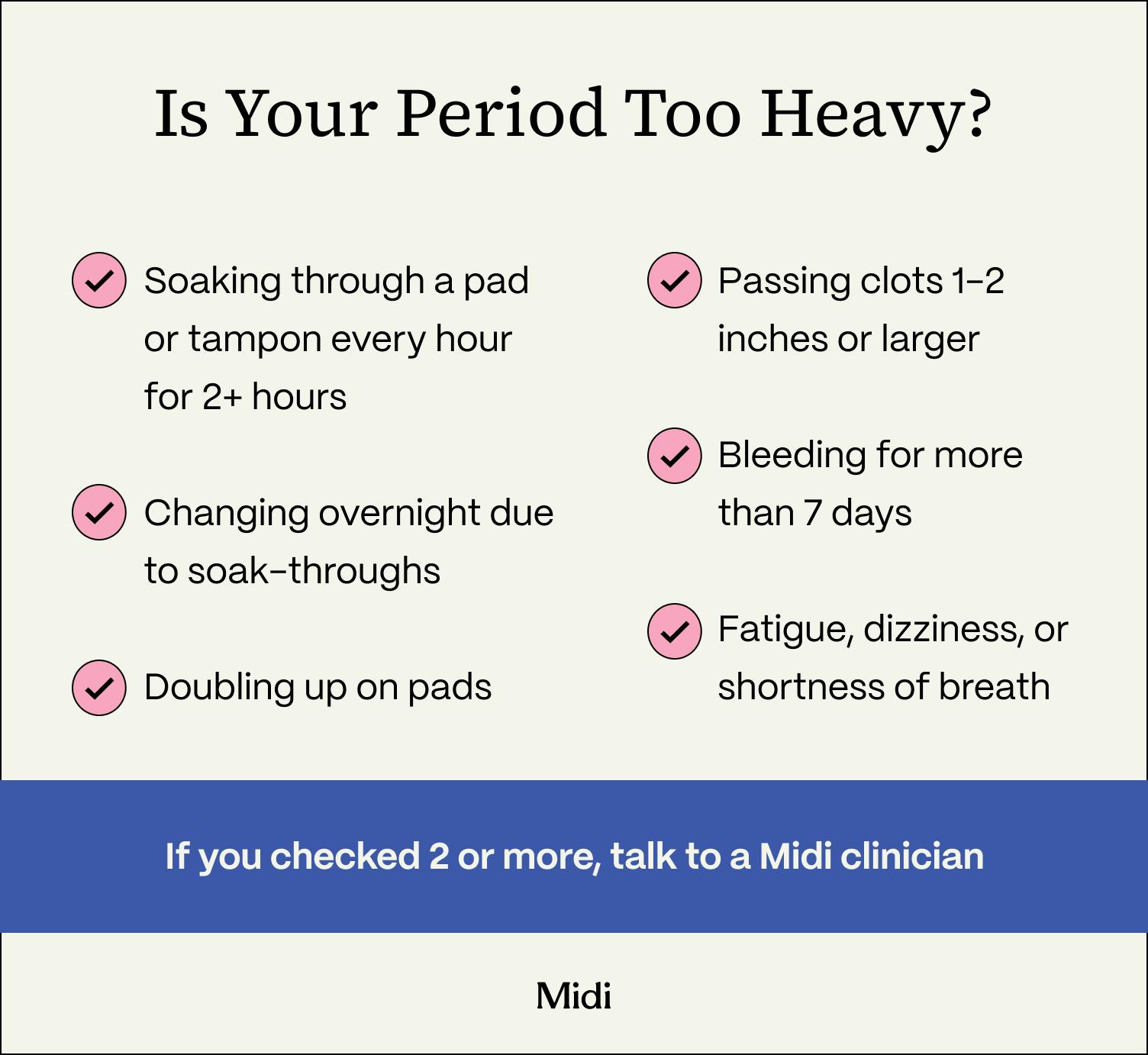
Signs you’re losing too much blood during your period include:
- soaking through a pad or tampon every hour for 2 or more hours in a row
- changing pads or tampons overnight because of soak-throughs
- doubling up on pads to control your flow
- passing blood clots that are 1 to 2 inches or larger
- bleeding for more than 7 days
- having symptoms of anemia, such as fatigue, dizziness, or shortness of breath
If any of these signs sound familiar, it’s worth paying closer attention.
A heavy period shouldn’t be confused with spotting during menopause or other bleeding between periods. Spotting is usually lighter and shorter, and it might not even need a pad or tampon. Period bleeding, including clots, is typically heavier and lasts longer than spotting.
Why Is My Period So Heavy After 40?
Heavier periods in your 40s are often tied to perimenopause, but hormones aren’t the only factor. Certain conditions, medications, and other health issues can affect how heavy your flow is, and more than one cause may be at play.
Hormonal Changes During Perimenopause
The road to menopause can be rocky at times, especially as your periods become less predictable. One month it’s heavier, the next it’s lighter, and the month after it may not show up at all.
You can thank fluctuating estrogen and progesterone for that. Both hormones decline over time, but not all at once. During perimenopause, irregular ovulation means there’s less progesterone to balance estrogen, so the uterine lining can build up. When that thicker lining sheds, your period may be heavier and include clots.
Changes like this can feel unsettling, but they don’t automatically mean something is wrong.
“Around 40 is when perimenopause really starts, and periods can change a lot,” says Midi Health clinician Sonya Carothers, APRN, PhD, FNP. “You might see heavier bleeding and more clots, and that can still be a typical period for you.”
Structural Causes
Physical changes in the uterus can also cause heavy periods with clots.
Fibroids and polyps are typically noncancerous growths in or around the uterus. Fibroids grow in the uterine muscle, while polyps form in the uterine lining. Depending on where they are and how big they are, both can make periods longer or heavier, and may include clots.
With adenomyosis, the endometrial tissue grows into the uterine muscle, often causing painful or heavy periods.
Medical Factors
Sometimes, a heavy period with clots can point to an underlying health issue.
Thyroid disorders, for example, can throw your period off track. The thyroid is a small gland in your neck that helps regulate everything from your metabolism to your menstrual cycle. An underactive thyroid (hypothyroidism) has been linked to heavier or irregular periods.
Bleeding disorders like Von Willebrand disease make it harder for your blood to clot and can lead to heavier or longer periods.
Medications
Certain medications can also make your period heavier or harder to manage:
- Copper IUD: While hormonal IUDs typically have the opposite effect, copper IUDs may cause heavier, longer, or more painful periods, especially in the first few months after insertion.
- Missed hormonal pills: Forgetting to take birth control pills––which can happen to the best of us––can trigger breakthrough bleeding or spotting. Depending on how many pills you miss, you might also have withdrawal bleeding that feels like a heavy period.
- Blood thinners: Blood thinners (anticoagulants) make it harder for your blood to clot, which can result in heavier periods.
Pregnancy-Related Concerns
Even though ovulation is less predictable as you get older, you can still get pregnant during perimenopause. In some cases, heavy bleeding with clots may be related to pregnancy. An early miscarriage can look like a heavy period, with more cramping, clots, or tissue than usual. If there’s any chance you could be pregnant, take a test and check in with your OB/GYN.
Are Jelly-Like Blood Clots During Your Period Normal?
Small, occasional jelly-like blood clots during your period can be normal, especially on heavier days. During your period, your body naturally forms clots to help manage bleeding. Those clots usually break down before you ever see them.
But when your flow is faster or heavier, blood may briefly pool in the uterus, leaving less time for clots to dissolve before they pass. So you might see small, jelly-like clots during your period. They don’t automatically mean there’s a problem.
It’s a different story when period changes start to follow a pattern. Heavier bleeding over time, larger or more frequent clots, and persistent symptoms like dizziness or shortness of breath can signal that something else is going on. It’s important to check in with a healthcare professional, like a Midi clinician, who can help you figure out what’s causing the changes.
Self-Check: Track, Test, and Triage
If your periods have gotten heavier with more clots, a little tracking goes a long way. Start by tracking two cycles to see if you notice any patterns or worsening symptoms. You can use an app, digital calendar, or journal to note:
- how many pads or tampons you use per hour
- the number and size of any blood clots
- cramps, bloating, or pelvic pain
- symptoms like dizziness, fatigue, or shortness of breath
- missed birth control pills, new medications, or other possible triggers that can affect your cycle
Consider taking a home pregnancy test if there’s any chance you could be pregnant. Early pregnancy loss can look like a heavy period with clots, so it’s important to seek immediate care if the test is positive.
Heavy bleeding can drain your iron over time. If you’re feeling unusually tired or lightheaded, ask your clinician whether it makes sense to check your iron levels. While you wait for the test results, try adding more iron-rich foods, like leafy greens or red meat, to your diet.
Diagnosis and Treatment Options
A healthcare professional can help you figure out what’s causing persistent heavy periods with clots. Your visit might start with a conversation about your last few cycles, symptoms, and current medications. Based on your symptoms, you might need a pelvic exam or an ultrasound to check for fibroids or polyps. Your clinician may also order blood tests to check for anemia (CBC/ferritin) or thyroid problems.
That probably sounds like a lot of testing. But ongoing heavy periods after age 40 shouldn’t be dismissed, even if initial exams or blood work come back normal. It’s not fair to write symptoms off as “just perimenopause” without a closer look at what’s going on, says Dr. Carothers. Even virtual clinics, like Midi, can refer you for in-person care to get necessary screening tests.
Then, you can work with your care team to decide on treatment options. There’s no one-size-fits-all approach. Your treatment plan will be based on what’s causing the heavy bleeding and how severe it is. But it should also take into account your fertility goals and personal preferences. The goal is to create a shared plan to manage the bleeding, restore iron levels, and ease pain, so heavy periods don’t keep happening.
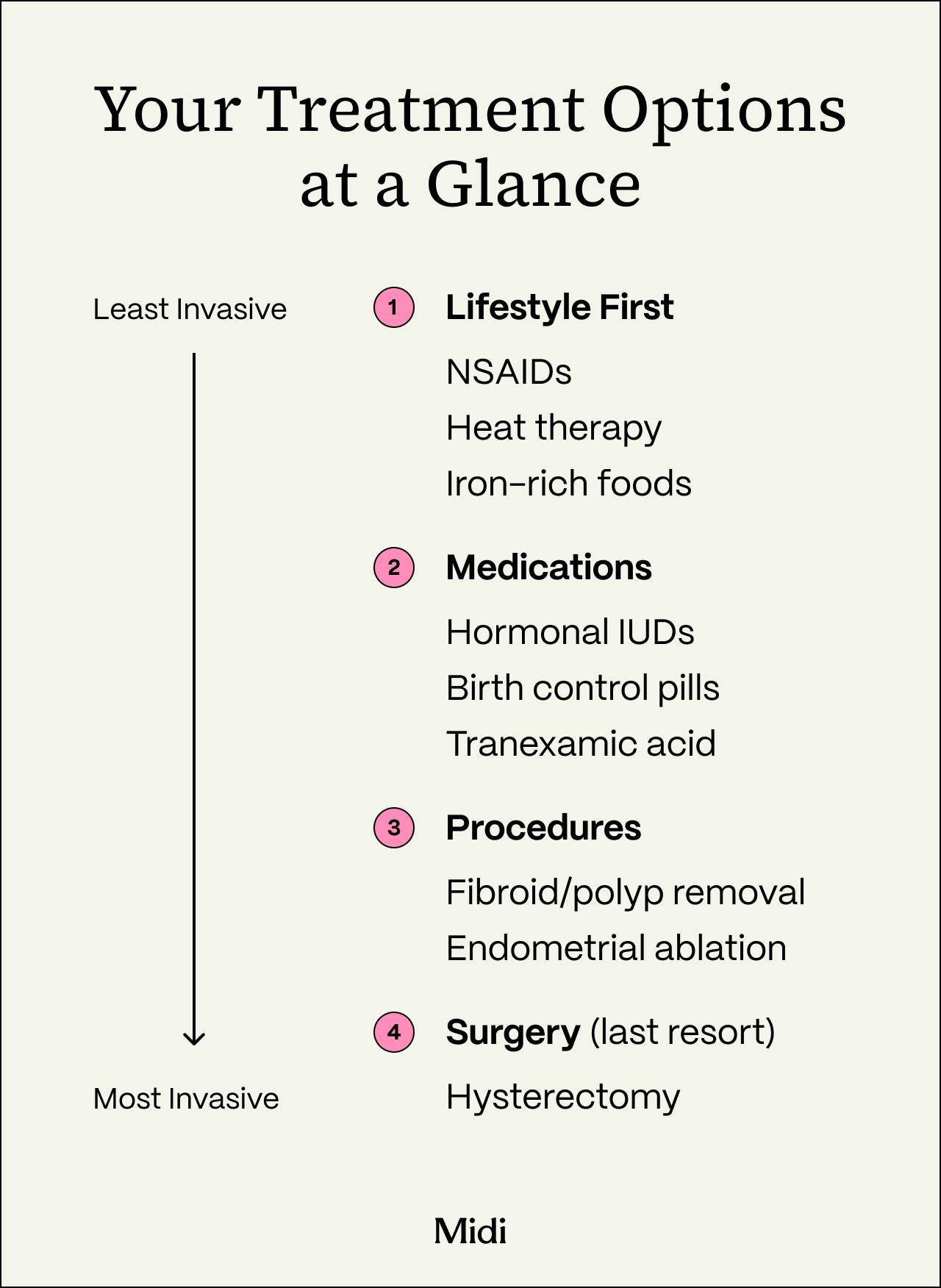
Non-Surgical Treatment Options
You may be able to manage heavy periods without surgery. Medications and lifestyle changes can reduce bleeding and make heavy flow days easier to handle. The right approach depends on your needs and may involve more than one treatment.
Lifestyle Support
It might surprise you that simple strategies can help with heavy or painful periods. If it’s safe for you, taking nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen regularly on your heaviest period days may reduce blood flow and cramps. You can also try heat therapy, like a heating pad or warm bath, to relax your muscles and soothe cramps. Other self-care strategies, such as staying hydrated and getting plenty of rest, won’t stop heavy periods with clots, but they can help you get through difficult days.
Iron Repletion
Over time, heavy periods can lower your iron levels, causing fatigue, dizziness, and shortness of breath even if you aren’t anemic. Rebuilding your iron might start with small lifestyle changes. A multivitamin or a diet that’s high in iron can be helpful, says Dr. Carothers.
Your healthcare professional may recommend:
- eating more iron-rich foods like red meat, leafy green vegetables, beans, and lentils
- pairing iron-rich foods with foods high in vitamin C––like tomatoes or citrus fruits––to boost absorption
- taking an iron supplement (with a stool softener or other treatments to reduce side effects)
Hormonal Treatments
Hormonal options are often used to treat heavy periods. They have been shown to regulate cycles and stop the uterine lining from getting too thick, which can reduce heavy bleeding. That could mean lighter, more manageable periods over time. The right option depends on your symptoms and fertility goals.
Common options include:
- hormonal IUDs (levonorgestrel)
- combined hormonal methods like the pill, patch, or ring
- cyclic or continuous progestin therapy
Non-Hormonal Prescriptions
If hormonal treatments aren’t a good fit, there are some non-hormonal prescriptions that can lessen heavy period bleeding. Tranexamic acid, for example, helps blood clot, which can lower menstrual blood loss. One study found that it reduced bleeding by about 40% to 50% and improved well-being in women with heavy periods. But your clinician will review your medical history, including any history of blood clots, to make sure it’s safe for you.
Surgical or Procedural Options
Heavy periods after age 40 don’t usually require surgery. But if you have severe or ongoing bleeding that doesn’t get better with medication, your healthcare professional may suggest surgical procedures.
Common options include:
- Polyp or fibroid removal: If benign growths in or around the uterus are responsible for your heavy periods, targeted procedures—such as a hysteroscopy or myomectomy—can remove fibroids or polyps while preserving the uterus.
- Endometrial ablation: This procedure breaks down the uterine lining to reduce heavy bleeding. Typically, it’s recommended only if you are done with or do not plan on having children, because pregnancy after ablation is not safe.
- Hysterectomy: A hysterectomy to remove the uterus is the most definitive option for heavy bleeding because it stops your period permanently. It’s usually considered only when more conservative treatments fail or bleeding takes a significant toll on your quality of life (if you don’t have your ovaries removed during this procedure, you will still experience menopause symptoms at roughly the same age as you would normally).
Your doctor can help you weigh the benefits and risks of each option, including effects on fertility and recovery times, to decide which one makes sense for you.
Working with a Healthcare Professional
It might feel awkward or hard to describe heavy periods with clots to a medical professional. But trust us: They’ve heard it all. And coming prepared and open to discussion can make your visit easier and more productive.
Bring your bleeding tracker, a list of medications and birth control you're taking, and any information you have on your family history of blood clots or bleeding disorders. It also helps to share your main health goals, whether that’s relieving specific symptoms or preserving fertility. Don’t be afraid to ask questions about likely causes of heavy bleeding, first-line treatments, and the best ways to monitor iron levels.
Before you leave, try to agree on a clear follow-up plan with specific, measurable goals––like fewer horrifying soak-throughs during your periods!––and when to check in again.
When to Seek Care
While heavy periods with clots aren’t always a red flag, some symptoms require urgent medical attention. Profuse bleeding that soaks through your clothes is an emergency and needs immediate care, says Dr. Carothers.
Get medical care right away if you experience any of the following:
- soaking through a pad or tampon every hour for 2 or more hours in a row
- passing very large blood clots, around the size of a golf ball, repeatedly
- dizziness, fainting, or a racing heart
- severe pelvic pain, especially on one side
- a fever
- any foul-smelling discharge
- a positive pregnancy test with heavy bleeding or shoulder-tip pain
- Any bleeding after menopause (new onset of bleeding after 12 months without a period)
This isn’t a definitive list. If anything about your period feels worse or different from your norm, it’s good to trust your instincts and check in with a healthcare professional.
Pain and anemia relief while you wait
Feeling dizzy, weak, or faint on heavy period days is a major sign that you’re losing too much blood, says Dr. Carothers. That much blood loss can lead to low iron or anemia, which is why it’s so important to get blood work if these symptoms keep happening.
While you wait for testing or results from your doctor, self-care measures can help on heavy period days, including:
- taking NSAIDs with food on your heaviest days, if it’s safe for you
- eating foods rich in iron paired with vitamin C, like spinach with oranges
- using heating pads or gentle movements to ease cramps
- getting restful sleep to reduce fatigue
- staying hydrated and limiting alcohol on your heaviest days
Key Takeaways
- Heavy periods after 40 with clots are common in perimenopause. Fluctuating estrogen and progesterone can make periods heavier, longer, and more unpredictable.
- Hormonal changes can lead to clotting. Less progesterone allows the uterine lining to thicken, causing heavier bleeding and visible clots when it sheds.
- Large or frequent clots aren’t normal for everyone. Passing clots larger than 1–2 inches or soaking pads hourly may signal excessive blood loss or anemia.
- Not all causes are hormonal. Fibroids, polyps, thyroid disorders, medications, and bleeding conditions can also cause heavy periods after 40 with clots.
- Tracking changes helps guide care. Flow, clot size, cycle length, and other symptoms are crucial pieces of information to share with your healthcare provider.
Frequently Asked Questions (FAQs)
Can perimenopause cause heavy periods with blood clots?
Yes, during perimenopause, estrogen and progesterone fluctuate from one cycle to the next. Ovulation becomes irregular, and the uterine lining thickens, causing heavier periods with clots.
What does it mean when your period is heavy and clots?
Heavy periods with clots usually mean your body is shedding a thicker uterine lining, which can make blood flow faster and heavier than usual. Small, occasional jelly-like clots can be normal, especially on heavy period days. But check in with a healthcare professional if you notice larger, more frequent clots or heavier bleeding. These changes may be linked to fibroids, polyps, or other medical conditions.
Why do I have clots in my period after 40?
After age 40, hormonal changes during perimenopause often explain why periods get heavier or have more clots. Structural issues like uterine fibroids or polyps and medical conditions such as thyroid or bleeding disorders can also play a role.
How do you treat perimenopause heavy periods flooding?
Treatment for heavy bleeding during perimenopause depends on how severe your symptoms are and how much they affect your daily life. Many people find relief with non-surgical options, such as NSAIDs (like ibuprofen), hormonal IUDs, and non-hormonal prescription medications. A healthcare professional may suggest that you consider procedures that can address fibroids, polyps, or other issues if more conservative treatments don’t help.
When should you go to the hospital for heavy menstrual bleeding?
Seek urgent medical care if you’re soaking through a pad or tampon every hour for 2 or more hours, passing very large clots repeatedly, feeling faint or dizzy, or noticing a racing heartbeat. Severe pelvic pain, fever, foul-smelling discharge, or heavy bleeding with a positive pregnancy test also require prompt evaluation. Any vaginal bleeding after menopause (12 months without a period) should also be checked right away.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered. Learn more here.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.

 Amanda Alvelo-Malina, MD
Amanda Alvelo-Malina, MD