Hormone pellets are a type of hormone replacement therapy (HRT) that are inserted under the skin and release hormones over a 3-6 month period. While they offer convenience and symptom relief for some women, including increased libido and energy, there are concerns about their safety due to lack of FDA approval and potential long-term risks. Many doctors, including those on the Midi Health medical advisory board, advise caution when considering hormone pellets.
Let’s be honest: When you first hear the word “pellets,” you’re probably imagining something you might feed a kid’s pet gerbil. You’re probably not thinking about a Tic Tac-sized form of medication that’s placed under the skin. But that’s exactly what hormone pellets are—they’re a type of under-the-skin hormone replacement therapy (HRT) that can last for three to six months to treat persistent menopause symptoms.
These days, there’s a lot of chatter on social media about hormone pellets. Some women swear by them. Many doctors are wary of them. There’s also a lot of debate about the efficacy and safety of hormone pellets (we’ll get into all that below). Still, some women are drawn to the set-and-forget-it appeal of hormone pellets, because you only have to think about your treatment once every few months, making it potentially attractive to those of us who space on taking our birth control pills or fall asleep with a full face of makeup on. Not only are they convenient, but they can appear to work very quickly.
That’s likely why at Midi Health, we regularly hear from women asking if hormone pellets are an option they should consider. “When women are interested in pellets, it's usually because they haven't gotten the help they needed,” says Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine and the founding medical director of the Northwestern Medicine Center for Sexual Medicine and Menopause.
“When a woman first goes on pellets, she’ll feel amazing. Pellets will do that because they give you this huge surge of not only estrogen, but generally testosterone as well. And women's immediate reaction is, ‘Oh my God, I'm so happy I did this. Why didn't someone tell me about this sooner?’ But what they don't appreciate is that yes, you do get that initial surge of feeling wonderful, but, long term, pellets have not been shown to be safe.” And that initial burst of symptom improvement often doesn’t last with subsequent pellets.
That’s why many doctors, including the medical advisory board at Midi, don’t recommend hormone pellets to patients to treat common menopause symptoms.
Read on to learn more about hormone pellet therapy and what you should keep in mind before choosing this treatment option.
What Are Hormone Pellets, and How Do They Work?
Hormone pellets are one type of hormone replacement therapy. They’re small capsules—each roughly the size of a large grain of rice—that are implanted in your body, usually in the upper butt cheek or hip, by a healthcare professional.
The pellets then release hormones into your system. Often patients may be given a mix of estrogen and testosterone pellets (for example, one estrogen plus two testosterone pellets may be inserted to reach the desired dose). A mix of pellets is often prescribed to menopausal women once their estrogen levels have dropped to a certain level.
- Estrogen pellets: These are often suggested for someone not interested in taking testosterone or patients who have experienced negative side effects with testosterone. An estrogen-only pellet is one way to get a steady state of estrogen without having to take meds on a regular basis.
- Testosterone pellets: These pellets are often prescribed for women in perimenopause because their bodies are still making estrogen. A clinician might want to avoid the testosterone/estrogen combo because too much estrogen can lead to irregular bleeding, breast tenderness, bloating, and other side effects.
How Do You Use Hormone Pellets?
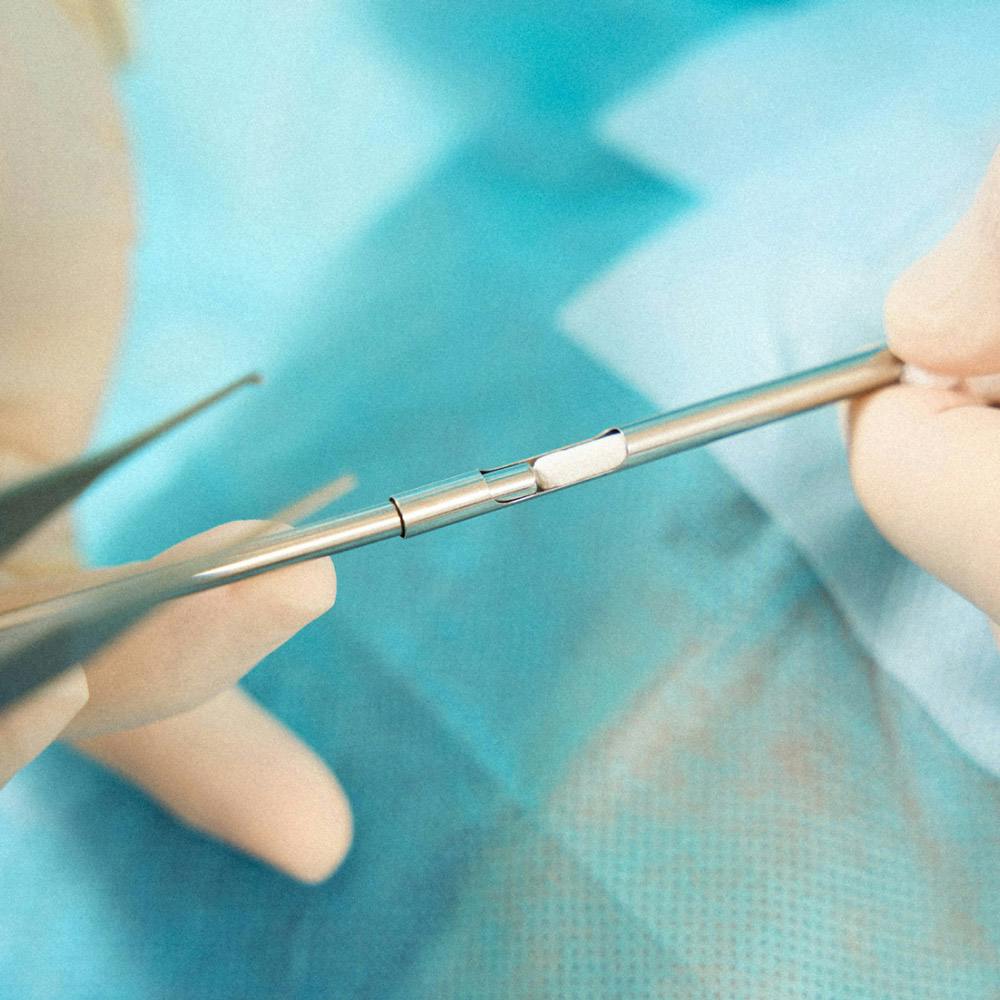
Unlike topical products, hormone pellets aren’t for the squeamish, as they’re inserted during a minor surgical procedure. The provider numbs your upper butt cheek or hip, then makes a small incision and inserts the hormone pellets; to close the incision, medical tape is used rather than stitches.
After the procedure, it’s usually recommended to rest and avoid submerging the area in water for 5-7 days. At that point, patients can remove the medical tape. Temporary side effects from implantation can include slight swelling, bruising, or redness at the incision site.
Does it Hurt to Get Hormone Pellets Inserted?
No, it shouldn’t hurt to have hormone pellets inserted. It may feel a little odd or uncomfortable, but the area is numb so you shouldn’t feel much at all, and it’s over very quickly. However some patients do experience “pellet extrusion” (in which the pellet is pushed out from its insertion position leading to a small, visible bulge), scars from the incision site, and scar tissue from repeated procedures in a similar area making future procedures more difficult.
What Is the Hormone Pellet Procedure Like?
It can be hard to picture what it’s like to get hormone pellets implanted under your skin. Here, one doctor walks you through her process:
Why Many Doctors Don’t Recommend Hormone Pellets
It should come as no surprise that many doctors aren’t too keen on prescribing a treatment that’s not approved by the FDA due to a lack of evidence for their safety and efficacy, especially when there are many better options available to women to treat their menopause systems.
“Long term, pellets have not been shown to be safe,” says Dr. Streicher. “Pellets are unregulated and haven’t been well studied. And you’re usually getting much higher doses of estrogen and testosterone than is needed in order to feel your best. As a result of this, one of the problems starting to crop up is an increased risk of uterine cancer and pre-cancer, because these very high levels of estrogen and testosterone can sometimes cause an abnormal buildup in the lining of the uterus.”
The lack of regulation means you have no way of knowing what you are getting, and studies have shown that the amounts vary regardless of “the prescription,” says Dr. Streicher.
And given that pellet therapy is a more aggressive form of HRT, your levels rise much faster and higher than with other forms of HRT. This opens the door to patients having a higher risk of experiencing other side effects than with other forms of treatment. These forms can include water retention, breast tenderness, facial hair, acne, and thinning of hair.
Another important thing to note: Once pellets are inserted there isn’t a way to remove them unless the provider goes in and opens the incision to look for them and then attempts to remove them. Because of this many patients are stuck with waiting out the 3-6 months for the pellets to stop working in order to get relief.
Midi’s Chief Clinical Officer, Mindy Goldman, MD, a practicing OB/GYN at the University of California, San Francisco (UCSF) for almost three decades who currently serves as the Director of the UCSF Gynecology Center for Cancer Survivors and At-Risk Women, shares why many in the medical community aren’t going to prescribe testosterone pellets:
But don’t just take it from us. Other doctors have weighed in on the problems with pellets:
What Are the Main Pros and Cons of Hormone Pellets?
There are, of course, upsides and risks to consider with any medical choice. When it comes to hormone pellets, there are some benefits and downsides you should be aware of and talk to your healthcare provider about.

Pros of Using Hormone Pellets Over Other HRT Methods:
The specific upsides to using using pellets versus other HRT deliveries are:
- Less mental load. The main perk of hormone pellets is that you only have to think about your HRT a few times a year because it’s a long-term option without having to think about it on a daily basis.
- Privacy. Unlike some HRT options (we’re looking at you, estrogen patch), which are visible, no one can see the hormone pellets under your skin, so the fact that you’re taking estrogen is only between you and your doctor.
Cons of Using Hormone Pellets:
There are some major possible downsides to using pellets, including:
- Difficulty finding the right dose. Usually you’re put on a low dosage of hormones at first and re-checked often until your provider determines you’re at the right level to make a difference in your symptoms. This can mean frequent lab visits for blood draws to check levels, and medical appointments to add hormone pellets. (You don’t want a too-high dose of estrogen or testosterone. Symptoms of too much estrogen include weight gain, fatigue, and mood swings, while too much testosterone can cause symptoms such as acne or oily skin, increased facial or body hair, hair loss, voice changes such as deepening of voice that can be irreversible, mood changes, and water retention.)
- Less flexibility to adjust or discontinue. If you don’t like how you feel using HRT pills, creams, or a patch, you can just stop and the hormone(s) will make their way out of your system. That’s not as easy with pellets. After a dose of pellets is inserted, additional pellets can be added, but they can’t be taken out, which means if you don’t feel great because your dose is too high, you’re stuck with it for 3-5 months until the effects taper off.
- Multiple surgical visits. Since the pellets are supposed to last for months, adjusting your dose may mean new incisions to add pellets to adjust your dose.
- Incision issues. These may include an infection, itchiness, or redness at the injection site and possible pellet extrusion (when the pellet pokes out of where it was inserted). Pellet extrusions can also cause localized infections, though in one study of over 376,000 patients who received hormone pellets, pellet extrusion only occured in less than 1% of women.
- Expense. One estimate is that pellet treatments have an average annual cost of $1,536, and most insurance companies are unlikely to cover pellets that are compounded bioidentical hormone therapy because they’re not FDA-approved. (Most insurers do cover FDA-approved forms of HRT, including patches, pills, and rings.)
- Unintended pregnancy. Pellets don’t protect against pregnancy. If you’re not using some form of birth control and become pregnant while on pellets, you risk exposing the fetus to extra testosterone and estrogen.
Why Would Someone Want to Use Hormone Pellets, Anyway?
Dr. Streicher says she gets the appeal of hormone pellets—patients do report feeling better on them which can be welcome relief after years of suffering. Your libido is up, you’re sleeping better, your hot flashes are calmed…what’s not to love? Why wouldn’t you want to stay on them forever? Well, that’s the issue. The short-term gain may not be worth the potential long-term pain of increased cancer risk.
“You want to see a clinician who is really going to be mindful of not just how you are feeling today or tomorrow, but how you are going to be feeling 20 years from now,” says Dr. Streicher.
And because hormone pellets last for several months, if you get the right dose (a big if, by the way), some patients like that they don’t have to think about HRT more than a few times a year, versus a daily or weekly treatment that can be easy to lose track of. But if you get the wrong dose that’s perhaps too high, you have to struggle through the side effects (like hair growth in places you haven’t had it before thanks to all the testosterone) for months before it can be regulated.
“We want you to feel good,” adds Dr. Streicher. “We have the same goal, but we want to do it in a way that has been proven to be not only effective, but also safe.” There are many other better options for HRT that check that box.
Who Is an Ideal Candidate for Hormone Pellets, and Who Should Avoid Them?
HRT in general, in the form of pellets or other interventions, may not be safe for patients with higher risk factors for heart disease, breast cancer, stroke, blood clotting disorders, uterine cancer, chronic liver issues, or migraines with auras. If you’re not in one of these high-risk groups, pellets still aren’t without their risks, including getting too-high dose or pellet protrusion.
To find out what HRT will work best for your body, goals, and lifestyle, it’s best to book an appointment with a Midi clinician.
How Hormone Pellets Stack Up Against Other Forms of HRT
Hormone pellets are hardly your only option for menopause symptom relief. There are many other FDA-approved forms of hormone replacement therapy that have been deemed safe. If you’re looking for a treatment that includes testosterone, Midi uses testosterone cream (or gel), which makes it much easier to control dosing, adjust as needed, and monitor for side effects.

What Is the Menopause Transition?
Before we dive into hormone pellets, we should back up a second here and start with what's going on in the body that would make someone consider having a medical professional insert little hormone Tic-Tacs into their body.
First, a crash course in your hormones. There are two main stages your body goes through as it prepares to reach the end of its reproductive years and put a cap on your periods and ovulation.
- Perimenopause, which usually starts when a woman reaches her mid 40s (though it can begin much earlier than that), occurs when the hormones estrogen and progesterone naturally begins to decline as you inch closer to the end of your reproductive years. During this phase, you may experience symptoms like hot flashes, night sweats, and mood swings, but you’re still getting your period and you’re still ovulating (though both will become less regular over time).
- Menopause isn’t actually a phase but a moment in time, marked by the pivotal point when you’ve gone a full 12 months without a period.
After you cross the menopause threshold, you’re considered postmenopausal, but symptoms can linger on for years as your body adjusts to its new hormonal normal.

12 Common & Surprising Symptoms of Perimenopause and Menopause
Some women may only experience a few symptoms during this transition, but, for most women—a whopping 85%!—this hormonal transition comes with serious side effects. And many women seek out hormone pellets to ease their suffering, plain and simple.
As your estrogen levels become erratic and slowly decline, nearly every system and organ in your body goes on a roller coaster…but not really the fun kind. Nope, it’s more like hormonal chaos that can cause problems for your sleep, your mood, your brain function, how you look, and how you feel. The list of symptoms from this hormonal temper tantrum include:
- Irregular periods: A change in your period is often the first sign of perimenopause, and women experience markedly irregular menstrual cycles as time goes on. Period variability usually lasts one to three years, until eventually, it stops entirely.
- Hot flashes: One of the most well-known symptoms of menopause, hot flashes bring on a sudden feeling of intense heat that might come with a flushed face, sweating, rapid heart rate, and wrap up with a cold chill. About 75% of women experience hot flash symptoms and they generally persist for around seven years, with a single episode lasting anywhere from one to ten minutes.
- Night sweats: A sister symptom to hot flashes, night sweats are simply hot flashes that happen at night. They can wake you from a sound sleep, drenched in sweat and kicking off covers for relief.
- Sleep Trouble: Difficulty sleeping affects 61% of menopausal women, and for those who experience hot flashes, nearly 44% suffer from chronic insomnia (anxiety and night sweats are one culprit there).
- Weight Gain: For a host of reasons (some hormonal, some not), metabolism slows down about 5-10% each decade. As a result, weight gain is incredibly common during midlife even if your lifestyle remains mostly the same. How much weight? Women gain about 1.5 pounds per year during their post-menopausal years. Hormonal changes also affect fat distribution and body composition, so weight gain concentrates in the upper body, particularly the abdomen (hello, meno belly).
- Mood Swings: As many as 70% of women deal with mood changes through the menopause transition. That can include overwhelming reactions to everyday events—anything from tiredness to tears to full-blown rage. Another 25% of women notice increased mood swings that can range from mild to severe.
- Vaginal dryness: Estrogen helps to keep the skin all over your body, but especially in the vaginal area, strong and well moisturized. So a decrease in estrogen means less vaginal lubrication, which may lead to vaginal dryness, thinning of the vaginal walls and less elasticity. All these can add up to pain with sex.
- Lower sex drive: Around 77% of postmenopausal women report low sex drive. Estrogen is directly connected to sex drive, so it’s no surprise that as the hormone dwindles during perimenopause and menopause, libido may drop along with it.
- Brain fog: About 60% of menopausal women report brain fog, described as difficulty remembering details—from names to appointments to common words.
- Itchy Skin: Estrogen helps to keep skin healthy by supporting the production of collagen and natural oils, as well as retaining moisture. Through the hormone transition, estrogen steadily declines, which means drier, thinner, and for plenty of women, itchier skin.
- Joint Pain: Estrogen helps to reduce inflammation, regulate fluid levels, and protect bones—and all those benefits keep joint pain at bay. As levels decline during the menopausal transition, achiness in your knees, shoulders, neck, elbows and hands might crop up.
- Incontinence: About 50% of postmenopausal women suffer from loss of bladder control (say, on the way to the bathroom) or involuntary urinary leakage that may suddenly happen with a sneeze or laugh. All these urinary issues are associated with hormonal changes that lead to loss of elasticity in the vaginal tissue, thinning of the lining of the urethra and weakening of the pelvic floor muscles.
In many ways, the menopause transition is not unlike puberty. But instead of ramping up to your reproductive years, you’re now ramping down. Unlike puberty, however, we have more and better tools for dealing these days than in our tween/teen years. There’s no need to take a grin-and-bear-it approach to menopause. There are many treatment options that can turn the transition from barely tolerable to liberating.
Symptoms can absolutely be treated and improved with options including lifestyle changes, supplements and herbal remedies, and hormone replacement therapy (HRT). Midi supports all of these, and works with you to make sure you feel confident about the choices you make. While HRT is the gold standard for improving and reducing the severity of most symptoms, it’s not right for every woman, so find a collaborative specialist or Midi clinician to individualize your treatment.
What Is Hormone Replacement Therapy (HRT)?
Hormone Replacement Therapy (HRT) has long been a go-to solution for managing many menopausal symptoms caused by hormonal fluctuation (sometimes mistakenly referred to as hormonal imbalances though your hormones are never technically balanced), particularly hot flashes and mood swings. The name is a little misleading—you’re not replacing any hormones but supplementing your estrogen levels.
HRT, sometimes referred to as menopausal hormone therapy or MHT, works by releasing bioidentical hormones (which means they have the same chemical and molecular structure as hormones that are produced in the human body) into the bloodstream or vaginal tissue. It is available in many forms, including pills, patches, vaginal rings, pellets, topical creams and gels. To protect the uterus (in patients who have one, as opposed to those who’ve undergone a hysterectomy), doctors add progesterone or progestin to estrogen, which reduces any risk of uterine cancer.
The best part is that HRT is effective at relieving menopausal symptoms. In fact, a large body of recent research shows that if women start hormone replacement therapy within 10 years of their last period, not only do they enjoy significant relief from menopausal symptoms but they also have a lower risk of heart disease and bone loss. HRT may also be connected to decreased risk of diabetes and weight gain.
There are two ways to treat symptoms through HRT:
- Systemic hormone therapy, a dose of estrogen that is absorbed throughout the body via pellet, pill, skin patch, ring, gel, cream, or spray; this can treat any of the common symptoms of menopause.
- Low-dose vaginal products, where a lower dose of estrogen is absorbed directly in the vaginal area through a cream, tablet, or ring form—but since less estrogen is absorbed by the body, it’s usually only used to treat the vaginal and urinary symptoms of menopause, so won’t help with brain fog or night sweats, for example.
The Takeaway
- Hormone pellets are a form of hormone replacement therapy (HRT) that are inserted under the skin (usually in your hip or butt area) and release hormones for 3-6 months.
- There are pros and cons to hormone pellets. Many doctors, including the medical advisory board at Midi Health, do not recommend hormone pellets because they aren’t FDA-approved and may pose health risks with long-term use.
- However, some women do tolerate hormone pellets well and like them for their set-it-and-forget-it convenience as well as symptom improvement, notably a boost in libido and energy.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.