Hormone replacement therapy (HRT), also referred to as menopausal hormone therapy or MHT, is widely considered the single most effective treatment for relieving some of the most stressful symptoms of perimenopause and menopause, including hot flashes, night sweats, vaginal dryness, and recurrent urinary tract infections. But is it right for you? And when should you start it? Those questions of course should be answered in conjunction with a knowledgeable healthcare professional, like a Midi clinician, but there are some telltale signs that you may need HRT. Here’s how to spot them, so you can get the help you need.
For Chicago attorney Wendy Steiner’s Saturday Night Live-themed 50th birthday party, she dressed up as Molly Shannon’s iconic Sally O’Malley character, known for kicking, stretching, and generally refusing to feel old while proudly proclaiming “I’m 50!” For the past several years, though, Steiner had been battling exasperating symptoms that made her feel less than enthusiastic about aging: fatigue, depression, achy joints, and night sweats that necessitated multiple pajama changes a night. Internet research pointed her toward the most likely culprit: perimenopause. She also learned about hormone replacement therapy (HRT) as a possible treatment. “I was reading about signs that you need HRT, and I checked off so many boxes,” Steiner says.
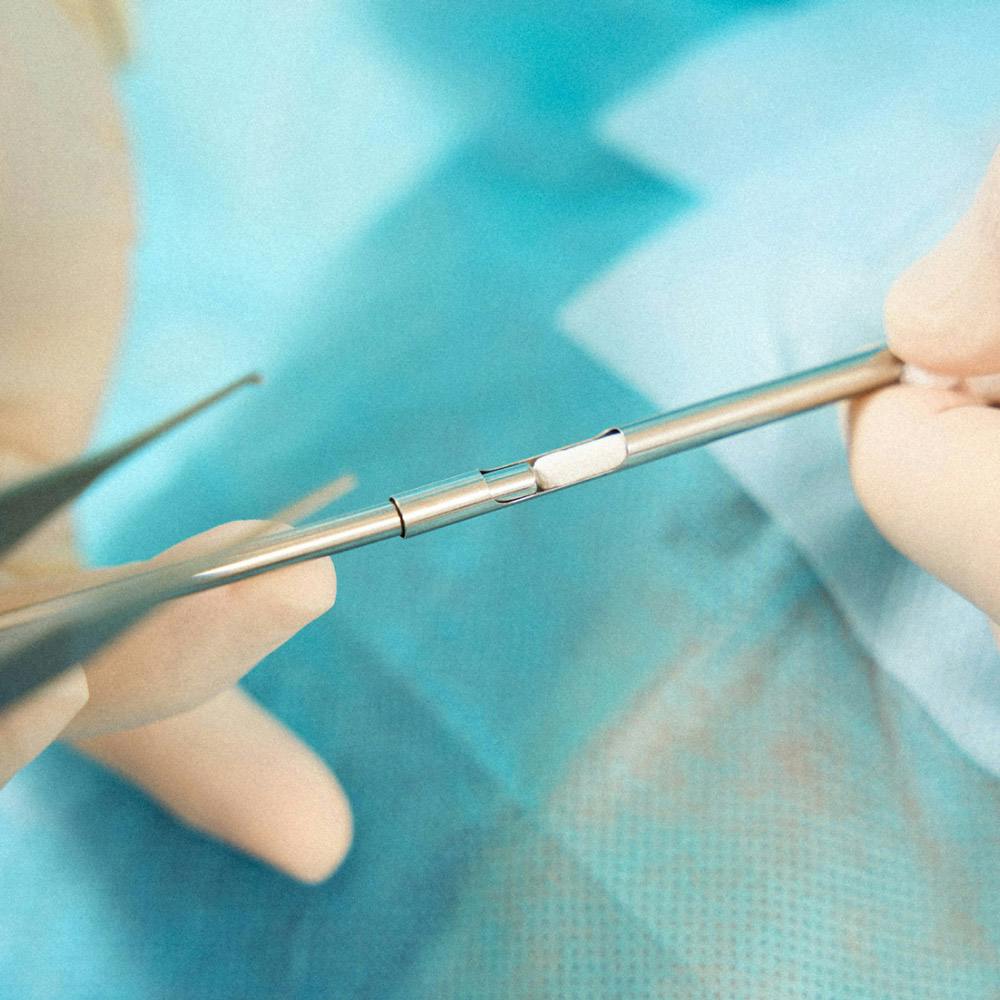
At her first Midi Visit, after discussing her symptoms, medical history, and current medications, Steiner’s Midi clinician suggested an estrogen patch and oral progesterone—awell-tolerated hormone therapy regimen designed to mitigate symptoms related to fluctuating hormone levels. Steiner noticed an improvement in two to three weeks. “My aches were less intense, my energy level was picking up, and I was sleeping better—my night sweats stopped.” Celebrating her 50th with her friends, Steiner rocked a red polyester pantsuit, bouffant wig, and her secret accessory: an estrogen patch on her lower abdomen.
What Is Hormone Replacement Therapy (HRT)?
In the years leading up to your final period—known collectively as perimenopause—your body undergoes a slew of physiologic changes that can result in everything from hot flashes and vaginal irritation to low bone mass and a shortened emotional fuse. With HRT, a combination of estrogen and progesterone (for women who still have their uterus) or estrogen alone (for women who’ve had their uterus removed) is used to help ease some of the more bothersome symptoms.
HRT is also recommended for women who hit menopause before age 45, either naturally or after having their ovaries surgically removed. (The average American woman enters menopause at age 51.)
Available in many forms, including pills, patches, topical creams and gels, and vaginal rings, HRT works by releasing hormones into the bloodstream or vaginal tissues. That said, the acronym “HRT” is somewhat of a misnomer. “The most common formulations do boost estrogen and progesterone, but the amount does not come close to fully replacing our prior levels,” saysMidi’s Chief Medical Officer Kathleen Jordan, MD. But it’s so powerful that adding back just a tiny percentage of the hormones your body made during your peak reproductive years “is all that is needed to gain so many benefits,” she adds. Many experts now use the terms hormone therapy (HT) or menopausal hormone therapy (MHT instead). In this story, we’ll toggle between all three terms.
In the past 20+ years, a giant body of research has shown women who start HRT within 10 years of their last period not only enjoy significant relief from menopausal symptoms, but their future risk of heart disease, bone loss, diabetes, and weight gain improve, too.

6 Signs You May Need HRT
According to Dr. Jordan, three of the most widely agreed-upon clinical indications for HRT for women are:
- Hot flashes and night sweats
- Osteopenia, or lower-than-normal bone density (detected during a bone density scan)
- Irritating vaginal and urinary symptoms (such as vaginal dryness and recurrent UTIs) that interfere with sex drive, sexual satisfaction, and overall quality of life
We’ll cover these plus three other equally frustrating and life-altering symptoms that respond well to HRT.
#1: Persistent Hot Flashes and Night Sweats (Plus the Ensuing Insomnia)
Roughly 75% of women experience hot flashes and night sweats in midlife. When they hit during the day, they can be embarrassing and uncomfortable, sabotaging your ability to work and socialize. At night, they can make a solid night’s sleep feel impossible, the effects of which trickle down into nearly every arena of life, including cognitive functioning, mood and emotional regulation, heart health, and much more.
Experts aren’t clear why these hormone-influenced temperature surges detonate in midlife, but we know that estrogen influences the hypothalamus, the brain’s temperature-regulating headquarters. As estrogen levels fluctuate in perimenopause, the hypothalamus becomes more sensitive to even minor changes in body temperature and gets easily fooled into believing the body is overheated. In response, it enters “Cool Down” mode: Blood vessels near the skin’s surface expand; sweat glands spring into action. That would be great following a hard workout; in the middle of a work lunch, or at 2AM? Not so much.
Night sweats likely aren’t the only thing giving you nightmares. Here are other things keeping you up at night:
- Sex hormone fluctuations that directly impact the sleep-wake cycle
- Frequent nighttime urination
- Age-related sleep conditions like sleep apnea and restless leg syndrome
- Joint pain and body aches
- A mountain of stress
This perfect storm has nearly half of perimenopausal women, and up to 60 percent of postmenopausal women, saying their sleep is wrecked, per the Study of Women's Health Across the Nation (SWAN).

#2: Vaginal Dryness, Discomfort During Intimacy, and a Drained Libido
Vaginal tissue is rich with estrogen receptors. In our 20s and 30s, when estrogen levels tend to be juicy and consistently high, the skin of the vagina and vulva—as well as the skin lining the bladder and urethra (the tube that carries urine from the bladder to outside the body)—usually stays juicy and lubricated, too. But as estrogen naturally declines during perimenopause, these tissues can become dry, thin, and irritation-prone. The fallout can include vaginal itching and burning, painful intercourse (a.k.a. “sandpaper sex”), shrinking labia, increased nighttime wakenings to pee, and an increase in UTIs.
A checklist like that isn’t likely to put you in the mood for sex. Maybe that’s why 77% of post-menopausal women report low sex drive. A perimenopausal gradual drop in testosterone, a.k.a. “the hormone of desire,” may also be to blame; by the time you hit menopause, your testosterone levels are less than half of what they were at age 30.
#3: Mood Swings, Anxiety, or Depression
Estrogen calls plenty of shots when it comes to mood, teaming up with the nervous system to manufacture neurotransmitters like emotionally stabilizing serotonin and dopamine. As estrogen ebbs and flows in midlife, so do these mood-regulating brain chemicals, priming women for sadness and depression, anxiety, chronic overwhelm, anger, and mood swings.
Dr. Jordan points out that in addition to the direct effects of hormone changes, other irritating perimenopause symptoms, like insomnia, fatigue, and brain fog, can contribute to changes in mood. After all, it's hard to be happy-go-lucky when you're lying awake night after night and hot flashing in the middle of Costco.
#4: Irregular or Heavy Menstrual Bleeding
In your 30s, your periods may have been “Every-fourth-Tuesday-at-10AM” regular. Now, it’s a total crapshoot. “Your periods may be all over the place—close together, then far apart, some long, some short,” Dr Jordan says. “As you make less estrogen in perimenopause, sometimes you have enough hormones to ovulate, or release an egg, and sometimes you don't.” Ovulation is what sets the wheels in motion for regular periods. (Unless you get pregnant—a different story entirely!) To restate it all, in highly scientific terms: Irregular estrogen → irregular ovulation = hide-and-seek periods
Flow-wise, you may spot, or you might have what Canadian OB/GYN Jen Gunter, MD, author of The Menopause Manifesto, calls a “supersoaker event.”
In a study analyzing the menstrual cycles of 1320 multi-ethnic midlife women who participated in the SWAN Menstrual Calendar Substudy, 78 percent experienced three or more periods lasting longer than 10 days during their midlife menopausal years. The findings also suggest that during the menopause transition, more than one in three women will experience “bleeding that is so heavy they must change their sanitary products every one to two hours for four or more hours a day,” says study co-author Sioban Harlow, PhD, professor emeritus of epidemiology and obstetrics and gynecology at the University of Michigan School of Public Health.
#5: Cognitive Issues Like Brain Fog or Memory Problems
You know the thing that heats your food is called a stove. So why did you just call it a stapler? (And by the way…where on earth did you put the freakin’ stapler?!)
Before you book an appointment with a dementia specialist, know this: Estrogen promotes activity in the hippocampus, the memory and learning capital of the brain. As estrogen levels fluctuate in midlife, the hippocampus loses dependable access to the quantity and quality of brain fuel it’s used to, and the result might manifest as you losing your keys multiple times a day, spacing out on your aunt’s name, or completely forgetting to pick your kid up from school.
Additionally, midlife stress, mood changes, and shoddy sleep can also compromise memory and attention span. No wonder you have zero clue why you just walked into the kitchen.
#6: Low Bone Mass
Thirty-four million Americans have osteopenia, or bone density that is quietly weakening with age. Most of them are women in their 40s, 50s, and above. Diminished estrogen has its fingerprints all over this one, too—the hormone helps bones remain strong. Most women can expect to lose 10 to 20 percent of their bone mass during the 5-6 years around menopause, and a staggering 50 percent of women will break a bone due to osteoporosis—higher than your risk of heart attack, breast cancer, and stroke combined.
How HRT Can Help You
Adding a small dose of hormones back to your body in the years preceding and immediately following menopause can make a meaningful difference in how you weather the symptoms of perimenopause. It is considered the number one most effective treatment for relieving perimenopausal hot flashes, night sweats, vaginal dryness, and recurrent urinary tract infections, according to the most recent guidelines from The Menopause Society. HRT also can:
- Extinguish hot flash symptoms and insomnia by up to 90 percent.
- Slash fracture risk by up to 40 percent.
- Soften the impact of achy midlife joints, fatigue, weight gain, and much more.
You might even consider it a form of health insurance, as starting HRT within 10 years of your last period can reduce your future risk of several hormone-related chronic illnesses, like osteoporosis, arthritis, and heart disease, the number one killer of women.

Is Hormone Replacement Therapy Safe?
The Menopause Society, American College of Obstetricians and Gynecologists, Food and Drug Administration, and many other highly respected medical organizations say hormone therapy for women is safe when used appropriately. Dose, method (pill, patch, etc.) and timing (i.e., when you start taking it) are all important. At Midi, we support the responsible use of HT and will partner with you to find a personalized Care Plan based on your unique symptoms, risk factors, and wellness philosophy. When you book a virtual visit, your Midi clinician will determine whether HRT might be a fit, and explain the pros and cons.
Some women experience PMS-esque side effects like breast tenderness, bloating, mood swings, headaches, and irregular vaginal bleeding when starting HRT. Changing the dose or form of HRT (from a patch to a pill, for instance) may help.
Not everyone is a candidate for HRT
If you have any of the following, your clinician will suggest other, non-hormonal menopausal medications and treatments, such as nutrition changes, sleep hygiene, botanicals, and supplements, history of stroke or certain types of blood clots, certain types of heart or liver conditions, history of certain types of breast or uterine cancer, or current unexplained vaginal bleeding.
You don’t need to white-knuckle through your symptoms, so seek care from Midi or another provider with a deep understanding of the hormonal forces at play. Feeling better is within reach.
The Takeaway
- For many women, hormone replacement therapy is an effective way to treat the more vexing symptoms of perimenopause.
- There’s evidence that starting HRT within 10 years of your final period can also lower your future risk of heart disease and bone loss.
- Not everyone is a candidate for hormone therapy, depending on factors including medical history.
- Partnering with a skilled menopause-trained clinician can help you determine if HRT is right for you.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.


 Amanda Alvelo-Malina, MD
Amanda Alvelo-Malina, MD