If you've never experienced belly bloat, consider yourself lucky. Bloating is a common gastrointestinal issue during the menopause transition, caused by hormonal changes, stress, diet, or a combination of all three. Thankfully, you can battle bloating—with both prevention and treatment. Lifestyle changes, like exercise, key dietary adjustments, and avoiding triggers, can help. If you're still not finding lasting relief, a healthcare professional, like a Midi clinician, can help you identify possible causes and explore treatment options.
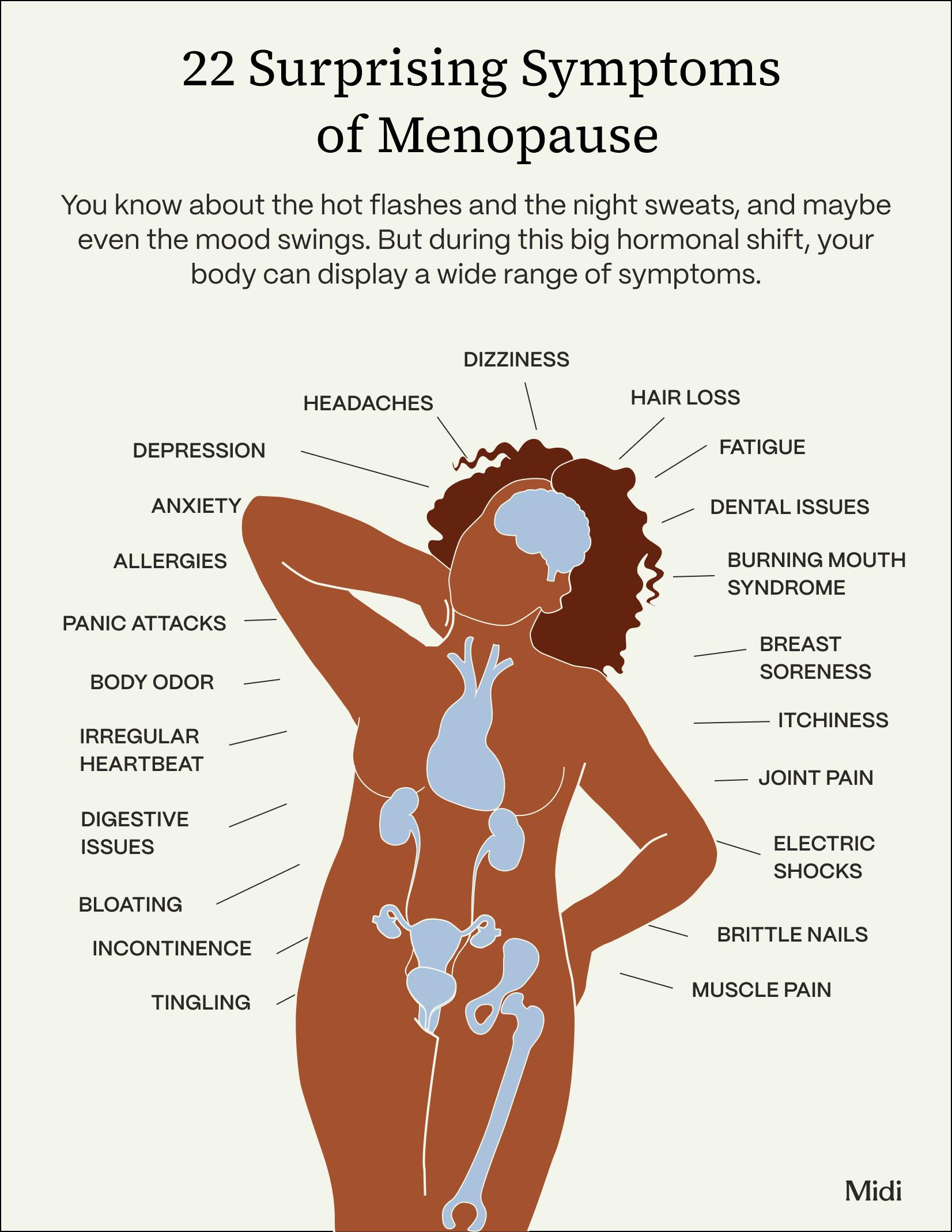
When you think of menopause symptoms, you may go to the most common offenders: hot flashes, night sweats, vaginal dryness. But the hormonal changes that happen in midlife can also bring on some really frustrating and uncomfortable gastrointestinal issues, including frequent menopause bloating.
Find out why it happens and, more importantly, the tweaks to your diet and lifestyle that can bring some much-needed relief (and get you back into your favorite jeans).
Understanding Menopause Bloating
What is Menopause Belly Bloat?
We often refer to bloating as that feeling we get when we eat too much and feel overly full, but bloating is actually brought on by gas build-up or water retention that leaves your belly distended and tight. It can be accompanied by other gastrointestinal issues, including:
- Nausea
- Stomach pain
- Irregular bowel movements
Bloating can be brought on by both the physical and psychological changes (hello, stress response!) your body goes through during menopause. A pretty unexpected symptom of menopause, it’s also uncomfortable, and contributes to just not feeling like yourself anymore.
Causes of Menopause Bloating

Why menopause can lead to bloating isn’t known for sure, but it likely comes down to these four factors:
Hormonal Changes
Fluctuations in estrogen are linked to gastrointestinal symptoms for all women (many notice that GI issues are linked to their menstrual cycle, ticking up at certain times of the month). So during menopause, when estrogen levels change dramatically, it’s no surprise that you’re at a higher risk for GI problems, including bloating.
Water Retention
Those changing hormone levels also directly affect water retention, which is when your body carries excess fluid. And there's some evidence that a drop in estrogen impacts how well your kidneys handle water, leading your body to hold on to more of it.
Inflammation
Something called gut permeability, or how much fluid and other nutrients make their way through the intestinal wall, increases as you go through menopause. The more permeable your gut is, the more inflammation you may have, contributing to GI issues like bloating.
Stress and Anxiety
Midlife can feel like a high-wire act, balancing work, family, friends, finances—along with major physical changes. Stress raises cortisol levels, creating a cascading effect in your body that can lead to gas and bloating. And anxiety can alter your breathing patterns so you literally swallow more air, which makes bloating worse.
Menopause Symptoms
Bloating isn’t the only gastrointestinal symptom you may notice during menopause. During midlife, women can experience more severe GI symptoms—such as diarrhea, constipation, stomach pain, and gas due to hormonal changes. Women with irritable bowel syndrome (IBS), defined loosely as having certain gastrointestinal symptoms without an obvious underlying cause, may also have more severe IBS symptoms during the menopause transition.
Managing Menopause Bloating
Unlike some health issues with a single treatment, reducing belly bloat during menopause may require a multi-pronged approach with some trial-and-error thrown in (so don't get discouraged!).
Here’s what can work, with tips from Midi clinicians, who help patients with GI challenges every day.
Dietary Changes for Relief
Because bloating is so closely linked to digestion, changing how you eat can have a big impact, whether you're in menopause or not.
Increase fiber intake.
“Maintain great gut health by eating a variety of quality fermented foods and fiber,” says Angela Orcholski, WHNP, ARNP, a women's health nurse practitioner and Midi clinician. Fiber acts as a "prebiotic," meaning it serves as food for the beneficial bacteria in your gut, allowing them to flourish and multiply by providing a source of nutrients that they can ferment and digest, which in turn helps maintain a healthy gut microbiome. “It may cause some extra bloating at first, but after the gut microbiome is functioning optimally, extra fiber in your diet will help create a healthy environment throughout the body,” says Orcholski. Make sure to increase your fiber intake slowly to reduce the risk that it will cause bloat in the short-term.
Maintain a healthy balanced diet.
Focus on eating well-balanced meals as often as you can. Nurse practitioner and Midi clinician Amanda Rosales, DNP, APRN, FNP-C, advises avoiding the usual suspects, like foods lower in nutrients, that can contribute to feeling overly full and abdominal discomfort. We're looking at you, candy, high-fat foods, and sugary sodas. “I tell my patients to avoid artificial sweeteners and processed food," says Rosales.
Consume smaller meals.
Try not to give your digestive system too much work to do all at once, so avoid eating large amounts of food in one sitting (you may need to eat more frequently, which is fine). And when you do eat, try to pull up a chair, relax, and chew slowly.
Consider supplements.
The best probiotics for women can be helpful when there is an imbalance in the gut microbiome, such as in the case of symptoms like bloating, says nurse practitioner and Midi clinician Kati Forholt, MSN, FNP, MSCP, but she recommends them only for short-term relief. "I recommend probiotics to patients on a temporary basis to help ease acute symptoms," she adds. Ideally, feeding the gut with proper prebiotics (like high-fiber foods), as Orcholski suggests, will help keep the microbiome balanced in the long run for more lasting relief. Another supplement to consider: ginger. "Adding a ginger supplement to your daily routine can also help reduce some feelings of fullness and abdominal discomfort," says Rosales.
Lifestyle Changes for Relief
Beyond tweaking your diet, these healthy habits can also make you feel better and ease belly bloat brought on by hormonal changes.
Incorporate regular physical activity.
Getting active any time of day will help with proper digestion and promote overall health, but it can also do wonders in the evening. “A 10-minute walk after dinner can aid digestion, help with gas and bloating, and also improve your sleep,” says Heather Cook, a family nurse practitioner and Midi clinician.
Find ways to reduce stress and anxiety.
This isn’t always easy to do, but see if you can manage your emotions in a healthy way throughout menopause—a time when life is throwing a lot at you. Physical activity can help here too, as can breathing exercises or meditation, talking with a licensed therapist, delegating daily tasks to others so you have more time for yourself, and spending time with close friends.
Know your triggers.
Some women may have more bloating after they eat dairy products, while others can notice it after drinking carbonated beverages. When you pick up on things that seem to increase that sensation of a tight, puffy stomach, take note and try to cut back. “Limit the consumption of foods, drinks, and medications that make your bloating worse,” says Lori Grant, a women’s health nurse practitioner and Midi clinician. “This can include over-the-counter medications like NSAIDs, antihistamines, and sleep aids, as well as supplements like calcium carbonate.”
When to talk to a doctor about bloating
If you have persistent, troublesome bloating you should bring it up with a healthcare professional, especially if you also have stomach pain, diarrhea, vomiting, bad heartburn, or dark/bloody stools.
Can HRT Help With Menopause Bloating?
Hormone replacement therapy (HRT) can help with many menopause symptoms, but bloating isn’t one of them. And in fact, HRT can make bloating worse (it’s mentioned as a possible side effect of HRT). One possible reason why: Higher levels of estrogen, like those experienced by women taking HRT, can lead to something known as gastroparesis, which is a slow-down in the digestion of food that can cause bloating.
That said, worries about bloating shouldn’t stop you from taking HRT—especially if you consider the benefits to both your other menopause symptoms and long-term health. A well-trained clinician can help you manage and adjust medications to find a just-right dose for you.
Menopause and Weight Changes
Bloating can sometimes be confused for true weight gain during menopause because the bloating (water and gas retention) can show up as a few more pounds on the scale—although that is different than change in body composition and weight that can come with menopause.
Simply put, menopause can be a time when many people do gain weight—in fact, 87% of Midi patients complain of weight gain and body changes. Women gain an average of 1.5 pounds per year in midlife; a study published in the International Journal of Obesity cited an average weight gain of 12 pounds within eight years of hitting menopause. The extra pounds are due partly to age and a decrease in lean muscle mass, but hormones play a role. One thing that can be blamed on menopausal hormone change is a shift in your body composition, with more fat accumulation around your midsection (aka meno belly).
At Midi, we understand that weight is a common challenge for women going through the menopause transition. Many of the hormone changes you experience as part of menopause are actually significant contributors to weight struggles.That’s why working with a healthcare provider to understand your hormone needs is important. Hormone replacement therapy, if it’s the right course of treatment for you, has the potential to set you up for success by addressing symptoms that make it easier to gain weight and harder to lose it. Remember: Any approach to sustained weight loss should be multifaceted, encompassing various elements that contribute to your overall well-being. So while diet and exercise are important, so is addressing hormones, reducing stress, and prioritizing sleep.
Living With Menopause Bloating
Menopause symptoms, and how long you experience them, varies greatly for woman, and that goes for bloating as well. That said, there is some evidence that complaints of GI issues including bloating peak for women in their 40s (when many are in perimenopause, the stage before periods fully stop). So postmenopausal women may see this annoying midlife symptom gradually fade away, but don’t just assume you have to suffer through. Talk with your healthcare professional about how you can proactively improve your gastrointestinal issues, because you deserve to feel your best during this phase, and every phase, of your life.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including vaginal dryness and irritation, brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.

 Amanda Alvelo-Malina, MD
Amanda Alvelo-Malina, MD