Vaginal itching during perimenopause and menopause is a common concern, often linked to hormonal changes or treatable infections. Understanding the cause is key to finding the right solution—whether it's addressing vaginal dryness from declining estrogen or managing an infection. With the right guidance, you can relieve itching through simple lifestyle tweaks, improved hygiene habits, and hormonal or non-hormonal treatments tailored to your needs.
Vaginal itching can be incredibly awkward and maddening. You can’t scratch, but you’ve got to scratch. You’re in public, or at work or in a million other places where reaching down there just won’t fly. So instead you shift and shuffle around in hopes that that will make a difference. (It won’t.)
If that’s an all-too-familiar urge, you may be dealing with menopause vaginal itching. It’s true that the normal hormonal shifts during the menopausal transition can cause a range of symptoms, including this one. (The hormonal roller coaster menopause sends our bodies on is truly incredible, and our vaginas are right with us on that ride.)
We’ll dive into why this happens, symptoms, and ways to manage it, including lifestyle changes and non-hormonal and hormonal treatments. Ready to squelch the scratch?
What’s Up with Menopause & Vaginal Itching, Anyway?
Menopause is sometimes talked about as if it’s a single day when a woman makes the transition from pre- to postmenopausal. (Cue the record scratch.) We know the reality is far from it. Menopause, a natural stage in a woman’s life, occurs when you haven’t had a period for one year. However, there’s an entire stage before that, and that’s called perimenopause, which lasts for four to six years–though for some women, up to a decade.
Perimenopause is the stage when you’re still getting periods (often irregular ones) but your hormones are starting to fluctuate, resulting in the symptoms of menopause. These symptoms—brain fog, joint pain, insomnia, and vaginal changes, and many more—differ for every woman. In this article, we’ll really hone in on vaginal itching.
Let’s start with the fact that these issues aren’t discussed enough. An overwhelming majority of providers don’t initiate conversations about vaginal symptoms with their patients and nearly three out of four women aren’t getting help for them, according to a 2020 UK study published in Post Reproductive Health. The good news is that Midi clinicians are well-versed in all things vaginal and know how to partner with you to find appropriate treatment. As you’ll read below, we have many solutions—it’s just a matter of identifying the right one.
Why Your Vagina May Be Itching
There are quite a few things that could be going on, some directly related to menopause, others made more likely by midlife hormonal changes, and a few more that have nothing to do with menopause at all. We’ll help sort it out.
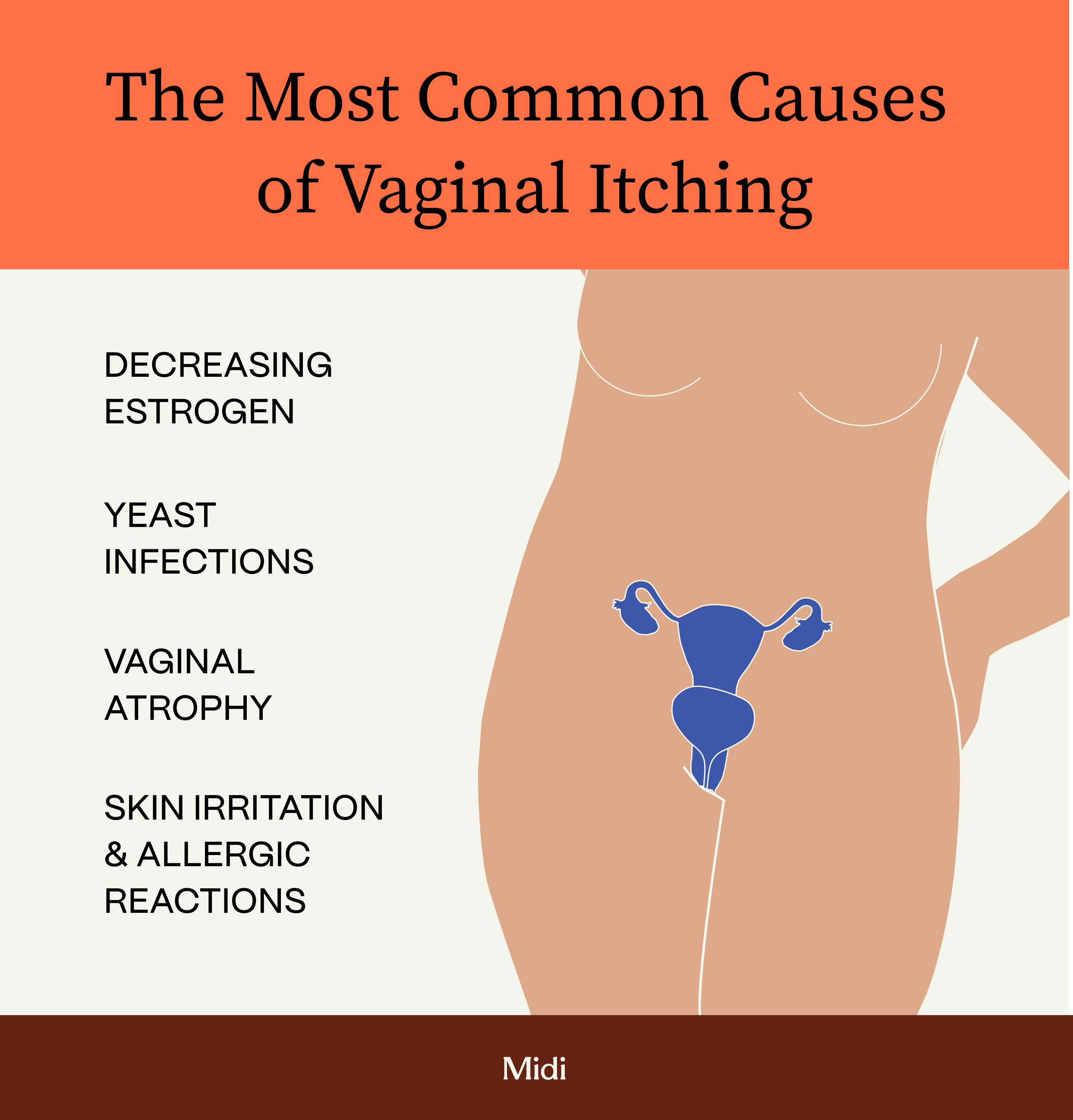
Decreasing estrogen levels
Simply put, our vaginas love estrogen. The hormone is what helps keep it nicely lubricated and elastic. The decrease in estrogen levels at midlife can cause us to experience vaginal dryness, itching, irritation, burning, changes in odor, and pain, according to research in Menopause, the journal of The Menopause Society. In this small study, which interviewed women aged 45 and over, one out of three reported vaginal itching. And we’re talking about more than a little itch here or there—these symptoms can impact our daily activities, sexual function, relationships, body image and self-esteem, among other consequences. One woman in the study above said that her itching was so bad, she had a tough time falling asleep.
Vaginal atrophy
As estrogen starts to drop in menopause, you can also experience what the medical community describes as “vaginal atrophy.” It’s a term that describes thinning and dryness of the lining of the vagina due to the estrogen depletion. (At Midi, we avoid using ‘vaginal atrophy’ language because it creates a stigma that can make it challenging to seek out care. We prefer genitourinary syndrome of menopause, or GSM, but you’ll likely encounter both).
The syndrome becomes more common throughout the menopausal transition, with 15% of women experiencing symptoms of atrophy—vagina dryness, burning, itching—before menopause and about half of women dealing with these symptoms after menopause. “Tissues of the labia and vagina are very sensitive to estrogen and suffer without it,” says Samantha Dunham, MD, an obstetrician and gynecologist and co-director of the Center for Midlife Health at NYU Langone Health. “But this is an area of physical change that will not get better on its own and definitely needs attention.”
Navigating Sexual Health During Menopause
Want more info about vaginal and sexual health during menopause? Watch this webinar for a ton of helpful facts and treatment options.
Vaginal infections & other conditions
- Yeast Infections. Three out of four women will have a yeast infection at some point in her life, and half will experience multiple episodes of them, according to the Office on Women’s Health.
Along with itching, you can also feel burning and notice a thick, white “cottage cheese”-like discharge. The good news is that your odds of having a yeast infection start to go down after age 57, though certain medications—including antibiotics, blood sugar-lowering drugs, and immunosuppressants—and conditions like diabetes can increase this risk, according to research in Current Infectious Disease Reports. Because estrogen affects yeast colonization, you may also be more vulnerable to a yeast infection if you are on hormone replacement therapy. If your clinician isn’t aware of this link, they may ignore the possibility of a yeast infection during postmenopause. It’s just another reason to make sure that your medical provider is well-versed in caring for women during and after menopause. - Bacterial Vaginosis. Another condition to have on your radar is bacterial vaginosis (BV). This is an imbalance between good and bad bacteria in the vagina. When “bad” bacteria proliferate and take over, you can be stuck with unusual discharge with a fishy odor, burning during urination, and irritation and itching. Changes in estrogen affect the “good” bacteria in our vaginas, and women are at risk for BV throughout the postmenopausal years and are sexually active, according to a 2022 study. Using a vaginal estrogen cream can help bring back a healthy vaginal microbiome and relieve symptoms.
Skin irritation & allergic reactions
Ever heard an OB/GYN say the vagina is like a “self-cleaning oven”? That’s in reference to the fact that your vagina typically maintains a balance in its microflora, but other factors, like hormonal fluctuations or washing with an irritating soap, can disrupt the vagina’s pH. When that happens, you may feel itchy. Dyes and fragrances in personal care products are another common source of skin irritation and itchiness, as well as vulvar dermatitis (a type of allergic reaction). Another culprit? Sitting too long in damp workout clothing or a wet swimsuit.
Symptoms of Vaginal Itching
Any type of vaginal or vulvar irritation can be associated with vaginal itching. Here’s what you might feel:
- Burning during urination
- Change in vaginal discharge
- Pain or discomfort with sex
- Vaginal dryness
- Vaginal itching, burning, or stinging
- Vulvar itching, redness, stinging, and swelling
How is Vaginal Itching Diagnosed?
Talk to your clinician. Yes, talking about the skin of your vulva and vagina can be uncomfortable. But so is the itching! And a conversation with a trusted clinician who understands the symptoms of menopause can be refreshing, reassuring, and lead directly to relief.
“There is a lack of medical training on female sexuality and age-related concerns, so it is important that women find a provider that’s open in discussing these concerns, is knowledgeable, makes a women feel heard, and validates her concerns,” says Midi’s Chief Clinical Officer Mindy Goldman, MD, who’s been a practicing OB/GYN at the University of California, San Francisco (UCSF) for almost three decades.
Your clinician should talk to you about your medical history, and you’ll be asked to describe your symptoms. If necessary, they may also recommend seeking out additional testing, such as seeing your gynecologist for a pelvic exam or to do testing for a yeast infection or BV. It is possible to have eczema or psoriasis on your genitals that flares up during menopause. A dermatologist will be the best expert to diagnose and manage these itchy, dry, flaky, rashy areas.
Finding Relief from Vaginal Itching

OTC & Natural Treatments for Vaginal Atrophy
The first place to look for ways to stop the itch? Over-the-counter options and simple, natural approaches:
- Over-the-counter creams, ointments, and suppositories: Products that improve vaginal moisture can counteract the dryness that causes itching. Midi clinicians recommend the vaginal moisturizing products by the brands Good Clean Love and Revaree by Bonafide. At the same time, there are also OTC vaginal anti-itch creams (i.e. those containing hydrocortisone) that can be applied topically on irritated areas of skin.
- Natural therapies: Sitz baths, or just sitting in a shallow amount of warm water, can soothe the area. Applying an ice pack (wrap it in a towel to safeguard your skin) can also help you find relief.
Medical Treatments for Vaginal Atrophy
When the more basic solutions you can try at home or pick up at a drugstore don’t soothe vaginal itching, there’s actually some good news: You have options. Vaginal atrophy could be the root cause, and the following prescription solutions are all on the table:
- Topical estrogen: Treating tissues with vaginal estrogen helps reduce dryness, inflammation, burning, and itching. Vaginal estrogen is available in a number of formulations, including cream, ring, or tablet. Some are designed to be inserted into the vagina, while other products are applied to the external vulva.
- Hormone replacement therapy (HRT): If you have additional symptoms of menopause, such as hot flashes or night sweats, HRT may be a good option for you. Not only can HRT reduce hot flashes by as much as 90 percent, it’s also been shown to eliminate symptoms of vaginal atrophy for 75 percent of women. HRT is not right for every woman, but having a thorough discussion with your clinician about all of your menopausal symptoms and your health background will identify the right treatment for you.
By the way, the name is a little misleading—you’re not replacing any hormones but supplementing your estrogen levels. HRT, sometimes referred to as menopausal hormone therapy or MHT, works by releasing bioidentical hormones (which means they have the same chemical and molecular structure as hormones that are produced in the human body) into the bloodstream or vaginal tissue. It is available in many forms, including pills, patches, vaginal rings, pellets, topical creams and gels. (Midi does not recommend pellets, however.) To protect the uterus (in patients who have one, as opposed to those who’ve undergone a hysterectomy), doctors add progesterone or progestin to estrogen, which reduces any risk of uterine cancer. - Non-hormonal prescription medications: Antihistamine and steroid medications may be recommended by your clinician to address severe itch, swelling, and irritation in certain cases.
Midi Patient Stories
Non-Hormonal Treatments for Vaginal Dryness
If itching is due to dryness, you’ve got an array of non-hormonal fixes to try on their own, or alongside an estrogen-containing solution. These are often recommended when sex is painful, so you’ll get less itching as a bonus if you try them for that sandpaper feeling during intercourse.
Vaginal moisturizers
These are topical products that target vaginal dryness. The idea is to use these all the time–not just to enhance an intimate movement.
It’s the same strategy as applying a lotion to your legs in the winter. Except these moisturizing products are designed to cater to the vagina’s pH and can be used safely in the vagina, whereas other skin lotions are not. Vaginal moisturizers are applied with an applicator inside the vagina.
Lubricants
Vaginal lubricants can be used prior to intimacy in order to add moisture to help make sex enjoyable again. Water-based lubes come in a wide range of consistencies and textures ranging from thin and slippery to thick, cushiony gel. Water-based lubes are compatible with all sex toys and condoms. However, water-based lubes tend to dry out quicker than silicone-based lubricants. Silicone is condom-compatible, tasteless and odorless. Silicone based lubes last longer on the tissues and can be used in the shower or bath. Just keep in mind: They’re a tad more expensive, may stain sheets, and may not be compatible with silicone based sex toys.
Vaginal dilators
Vaginal atrophy can make penetration during sex painful. This can happen not only because of dryness and lack of flexibility of vaginal tissues, but also because the vaginal canal can become shorter and narrower at midlife.
Vaginal dilators can help reverse these changes. Simple devices that you insert into your vagina, dilators slowly stretch the vaginal tissues and relax the muscles. You’ll start with the smallest device first and gradually work your way up to larger sizes. Finding a pelvic floor physical therapist can be incredibly helpful in guiding dilator treatment (and Midi clinicians refer patients for pelvic floor therapy frequently).
Natural oils
In general, you’re better off using products that are specifically designed for the pH of the vagina. However, oils like coconut oil may be an option as an alternative lubricant during sex. The catch: Oil is not compatible with condoms! Only use it if you are not relying on condoms for protection from pregnancy or STIs.
Taking Top Care of Your Delicate Skin During Menopause
Adopt Key Lifestyle Changes
- Maintain good vaginal hygiene: Wash your vulva with mild, non-irritating soap or simple plain water. Keep any products for external use only—don’t apply soap to the inside of your vagina, for instance. Avoid frequent baths, especially in water with scented soaps, as this can cause more irritation.
- Choose unscented products. Avoid using any fragranced products—body soaps, laundry detergents or dryer sheets, for example, or scented menstrual products like panty liners—on or around the folds of the skin of your vulva.
- Wear underwear with cotton gussets (the lining part that touches your vulva), which are gentle and moisture-wicking for this sensitive skin.
- Avoid tight fitting clothing: Tight, unbreathable clothing traps moisture, which can irritate your vulva. Change quickly out of sweaty workout clothes or wet bathing suits. Your vagina has to breathe, too!
- DON’T douche—it upsets the natural balance of the vagina, according to the American Sexual Health Association.
- Quit smoking: Nicotine use can stymie blood flow to the vagina, worsening symptoms like dryness. For cushy, flexible tissues, it’s important to maintain healthy circulation. It’s not lost on us that stopping smoking is a real challenge. Your clinician can provide resources so you can take the first step to quit.
When to Seek Medical Help
Vaginal itching can sound like a punchline, but it’s not a joke. Some women lose sleep over the discomfort and it can't do much for your sex life.
If you have vaginal itching and find an at-home or over-the-counter remedy that works for you, that’s great news.But if the itching persists or it goes away and then comes back, or it’s affecting your relationships, or making it difficult to go out and do everyday things, seek medical help from a trained clinician. Your quality of life matters too much to ignore this really common, and really fixable problem.
Frequently Asked Questions (FAQs)
How do you stop menopause itching?
There are many options for treatment for menopause itching. These include lifestyle changes, such as changing out personal care products and choosing fragrance-free formulas, to considering over-the-counter vaginal moisturizers or prescription medications like topical estrogen cream and, in some instances, HRT.
Can menopause cause itchy private parts?
Yes, the decrease in estrogen during the menopausal transition can lead to dryness, inflammation, and irritation of vaginal tissues, which affects more than half of women. These changes can cause vaginal itching.
What is the best cream for menopause itching?
This will differ for every woman, depending on why you’re itching in the first place. For some, an over-the-counter vaginal moisturizer can help. Others may benefit from topical estrogen therapy, such as a cream or ring, while some symptoms may be best suited for HRT. Non-hormonal prescriptions may also be appropriate.
The Last Word on Menopause Vaginal Itching
Menopause vaginal itching happens to a huge number of women, so there’s no need to feel alone in this experience. The vagina can go through a lot of changes as levels of estrogen decline at midlife. And it’s not just the urge to scratch that can be a problem, but other vaginal symptoms that tend to go along with itching, like dryness and discomfort during sex. It can feel intimidating to bring up vaginal issues with your provider, which is why most women don’t get the help they need and deserve.
Seek out a clinician that you feel comfortable opening up to, and one who you know will listen to your concerns. Finding a clinician you trust who is specifically knowledgeable in menopause—like those at Midi—can help you feel heard and understood, so you can access the right treatment to relieve your specific symptoms.
The Takeaway
- Vaginal itching during perimenopause and menopause is common—and can have a range of causes, from hormonal changes to certain infections.
- To zero in on the right treatment, it’s helpful to learn to tell the differences between itching that’s caused by hormonal changes and the kind of itching that may be a sign of a treatable infection.
- You can typically control the itching with some small but doable lifestyle and hygiene changes, as well as considering hormonal and non-hormonal solutions—topical and oral—that a knowledgeable clinician can walk you through.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including vaginal dryness and irritation, brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.

 Marissa Fontanez, DNP, FNP, FAIHM, MSCP
Marissa Fontanez, DNP, FNP, FAIHM, MSCP




