Nausea can be an unexpected and frustrating symptom of perimenopause and menopause, often tied to "sister symptoms" like hot flashes. Understanding how hormonal changes contribute to nausea can help you find relief through diet adjustments, natural remedies, Hormone Replacement Therapy, and non-hormonal prescription options may also offer solutions. Talking with a menopause clinician is the key to discovering what works best for you.
Hot flashes, night sweats, trouble sleeping. Sound familiar? They’re all common menopausal symptoms—but what about nausea? Can menopause cause that queasy feeling, too?
The short answer is yes. Sure, your nausea could be due to something you ate or a number of other issues, but if it’s a frequent unwelcome visitor, the culprit could be perimenopause.
Dramatic hormonal shifts during the menopausal transition can lead to nausea and a variety of other symptoms for women in midlife. Because nausea is less talked about, though, you may not have it on your radar at all.
And since it can catch you off-guard, it can be a confusing symptom. You may even ask yourself if you’re pregnant (hello, morning sickness?) or if this is actually another clue that you’re entering into perimenopause.
Are you Experiencing Any of These Other Menopause Symptoms?
During perimenopause, your hormones start doing a wild up-and-down dance. As the production of estrogen and progesterone fluctuate, women are often met with a variety–okay dozens–of what you can think of as ”sister symptoms.” Of course, these symptoms don’t all happen at once, and they won’t all happen to you (thankfully), but these erratic hormonal changes impact how you think and feel.
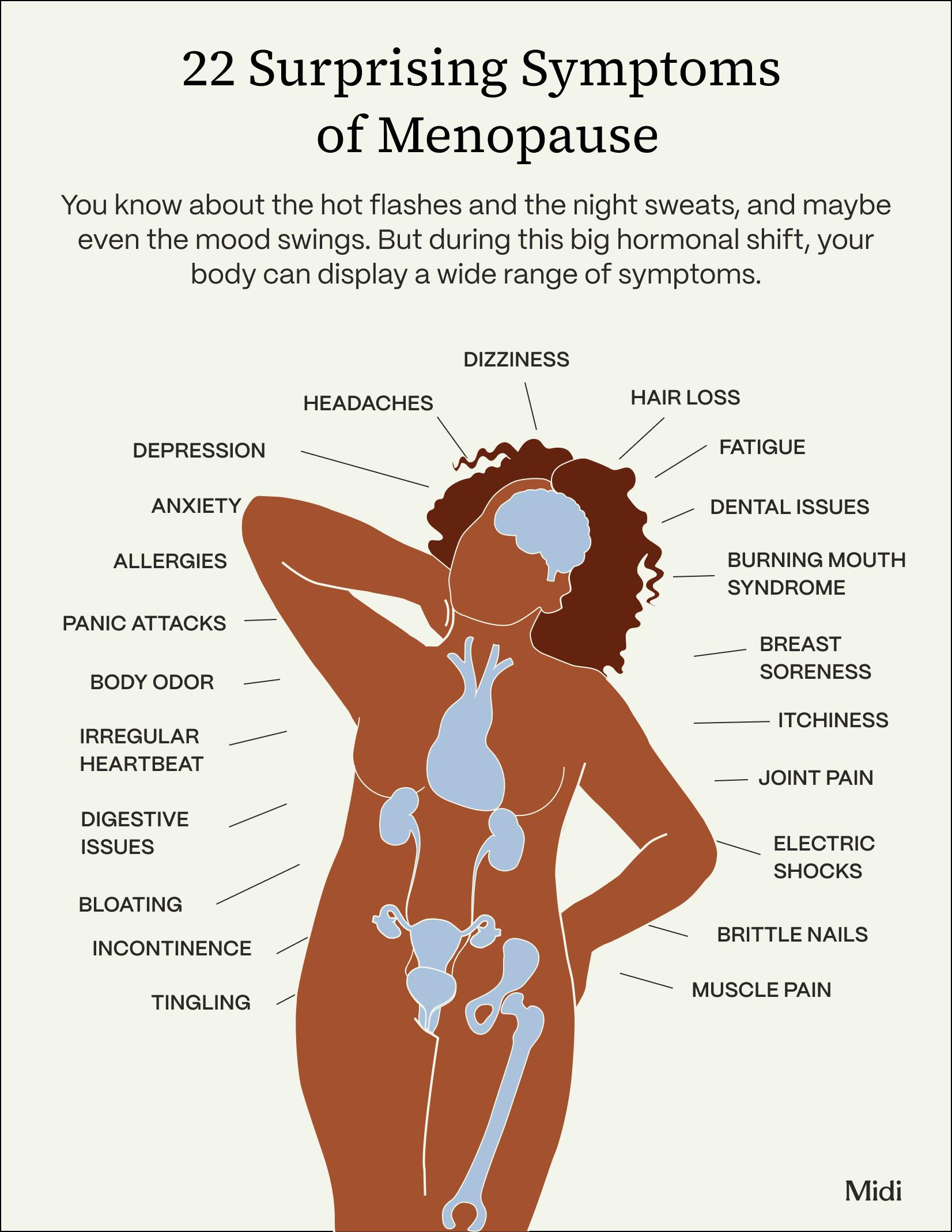
Some of the common—and surprising—symptoms of menopause include:
- Irregular periods
- Hot flashes and night sweats
- Sleep problems
- Mood changes and irritability
- Breast soreness
- Joint and muscle pain
- Vaginal dryness and decreased libido
- Brain fog
Menopause-Related Nausea: What’s Going On
At the most basic level, your body prefers to be even-keeled, especially when it comes to hormones. So when menopause throws things into chaos, you can feel nauseous. It’s similar to other times when your hormones may be out of whack, like during PMS or pregnancy.

These are the key “sister symptoms” most likely to lead to nausea:
- Do you have headaches and migraines? The pain of those can trigger queasiness.
- Dealing with hot flashes and night sweats? A small number of people report that their hot flashes also come packaged with nausea, according to research in the journal Menopause.
- Anxiety can also worsen hot flashes. And you know what tends to trot along with anxiety? Headaches and nausea.
- Some of the medications prescribed for menopause symptoms, including antidepressants, can cause nausea as a side effect. If you started on a new medication and are suddenly noticing nausea, it could be the Rx.
As you can see, many things could be going on that contribute to that sick-to-your-stomach feeling. Understanding your symptoms will help you get to the root cause so you can take action. Addressing nausea directly will help, but so, too, might stress management or medical treatments for menopause (more on both approaches below).
Managing Menopause-Related Nausea
If nausea is getting in the way of your day, here are some shifts in your daily routine that might clear the queasiness:
Make Diet Changes
Adjusting your eating habits to make sure that your meals and snacks are easily digestible can go a long way in navigating nausea. That includes decreasing the size of your meals, which will give your GI system the easier task of breaking down smaller amounts of food at one time. Aim for six or eight mini meals instead of three squares. Fat slows down digestion, so opt for low-fat foods and avoid fried or greasy dishes. Caffeine, alcohol, carbonated drinks, and spicy foods can also make you feel sick to your stomach. We’re all different, though. So if it helps, keep a journal of when nausea hits and what you were eating to see if you can sleuth out your own personal food triggers.

The Top Three Natural Remedies
Sometimes nature has the answer to your nausea. Here are three simple solutions to consider:
Ginger
One of the first things people reach for when dealing with nausea is ginger, and for good reason. A research review on women going through another hormonal fluctuation—pregnancy—shows that ginger can help reduce nausea. Whether you consume ginger (either as a food or supplement) on an empty stomach or after a meal, it may help improve the movement of food through the digestive tract, which improves nausea.
Peppermint
Mint may also help tamp down your nausea. In a study on cancer patients going through chemotherapy, those who applied one drop of peppermint oil on the spot between the upper lip and nose three times per day for five days reported less frequent and less severe episodes of nausea. If you don’t want to apply peppermint oil, you can also brew peppermint tea. You may find that inhaling the mint scent as you sip helps reduce queasy feelings.
Finally, many women get headaches and migraines when their estrogen levels take a dip, and these two can trigger nausea. Peppermint oil has also been shown to relieve migraine symptoms.
Vitamin B6
This B vitamin, pyridoxine, is used to treat morning sickness during pregnancy and it may come in handy again in this stage of life. B6 is an important component of anti-nausea medication—it may help produce neurotransmitters that, when lacking, contribute to queasiness. It’s also been found to relieve PMS symptoms in preliminary research. Take B6 in supplemental form, as well as eat foods like chickpeas, fish, poultry, fortified breakfast cereal, bananas, cottage cheese, and winter squash.
Managing Hot Flashes with HRT
If hot flashes seem to be at the root of your nausea, then Hormone Replacement Therapy (HRT) may be an MVP component of your treatment. “Hormone replacement therapy is statistically your most effective option and the quickest and most reliable path to symptom improvement,” says Midi Health Chief Clinical Officer Dr. Mindy Goldman, who is also Clinical Professor, Department of OB/GYN and Reproductive Sciences at UCSF. HRT is considered the gold standard to treat vasomotor symptoms (i.e. hot flashes and night sweats), according to the The Menopause Society. And it can can be incredibly effective, reducing hot flash symptoms by 90%.
Plus, HRT can also improve other aspects of your life that may be impacted by your persistent queasiness— such as better sleep, improved sexual function and libido, reduced cognitive fog, better skin health, reduced bone loss, and more.
By the way, the name is a little misleading—you’re not replacing any hormones but supplementing your estrogen levels. HRT, sometimes referred to as Menopausal Hormone Therapy or MHT, works by releasing bioidentical hormones (which means they have the same chemical and molecular structure as hormones that are produced in the human body) into the bloodstream or vaginal tissue. It is available in many forms, including pills, patches, vaginal rings, topical creams and gels. To protect the uterus (in patients who have one, as opposed to those who’ve undergone a hysterectomy), doctors add progesterone or progestin to estrogen, which reduces any risk of uterine cancer. Even if you’ve had your uterus removed, you might be prescribed progesterone, based on your symptoms.
Benefits and Risks of HRT
Just like any medication, HRT isn’t right for every woman. Plus, there are potential side effects that come with taking it. Ironically, one of those side effects is nausea, along with breast tenderness, irregular spotting, and changes in mood. If these side effects are severe or they interrupt your quality of life, speak to a trained menopause specialist, like those at Midi. There are options that allow you to stay on HRT, especially if it’s beneficial to other symptoms (like hot flashes and night sweats). If your hot flashes decrease but you’re still feeling nausea, your clinician may recommend a different form of HRT, to try to manage the hormonal fluctuations that could be at the root of your nausea.
Other Ways to Manage Hot Flashes
- Avoid triggers. If you give the brush off to irritating items such as alcohol, spicy foods, or hot beverages, you may find some relief.
- Consider certain supplements. “The most studied supplement in the treatment of hot flashes with demonstrated response rates is black cohosh,” says Dr. Goldman, “while several other supplements, such as siberian rhubarb and Maca root, also have evidence to support their effective use for hot flashes.” Keep in mind: with supplements and herbs it takes a longer time—as much as a month—to see the benefits. “And, as the response rates to these supplements are not as high as the prescription therapies, this approach often is best if trying one supplement at a time, each at least one month at a time, to see what might work best for you.”
- Look into non-hormonal prescription alternatives. According to Dr. Goldman, the best evidence is with venlafaxine, paroxetine, gabapentin or a newer drug to the market designed for hot flashes specifically: fezolinetant. These are especially useful for those who can't take hormones, perhaps due to a hormone receptor breast cancer for example, but also for those who may want to try nonhormone solutions.”
- Consider how you handle stress. You’ve been around long enough to know that stress is unavoidable, but it’s often how you respond to stressful situations—like maddening hot flashes!— that impacts how much you’re affected by them. Effective stress management strategies–yoga, mindfulness, talking to a friend, taking a break to breathe, heading out for a walk–are different for everyone. “Some women report improvement with acupuncture or mindfulness practices, while others really benefit from focusing on sleep, with environmental "hacks" such as cooling blankets and optimizing sleep hygiene practices,” says Dr. Goldman.
When Should You See a Doctor?
If your nausea comes and goes, is generally mild (though annoying) and your clinician thinks it could be one of your menopause symptoms, there is help. (There’s no need to grin and bear it when you’re feeling sick to your stomach!) Talk through your symptoms and how they’re affecting you, and weigh your options, whether those are lifestyle changes, medications like HRT, or botanical therapies.
Don’t discount other things that could be going on as well. You could be nauseous for many other reasons, like a GI infection, acid reflux, or as a side effect of a new medication.
If you have other symptoms like persistent vomiting, severe stomach pain, or you can't eat or drink, call your clinician or go to the ER.
Don’t Let Nausea Ruin Your Day
Nausea may often be an overlooked symptom of perimenopause, but that doesn’t mean it’s insignificant. Anyone who’s had a bout of belly churning knows that it can really derail your day, even preventing you from functioning. And you may not even know that the queasiness is connected to menopause, or that there’s anything you can do about it.
You can find help, either with a trusted clinician or by connecting with one through Midi. They can provide the support you need to help you get to the bottom of your symptoms and find the appropriate treatment for you. Along the way, you may find that many of the lifestyle changes you make to address your nausea also help ease other menopausal symptoms. And when it comes to feeling good day-to-day, that’s a win.
The Takeaway
- Nausea can be an unexpected symptom of perimenopause and menopause. While you might write it off as being caused by a million other things, a closer look could reveal that perimenopause is to blame.
- Some of the “sister symptoms” of menopause, including hot flashes, can lead to, or be accompanied by, nausea.
- Certain diet changes, a few natural remedies, and working to manage hot flashes (if you’re having them) can help you squelch the nausea. Also for hot flashes: A few non-hormonal Rx meds may be worth considering.
- Hormone Replacement Therapy (HRT) can be effective for hot flashes and the accompanying nausea. An in-depth discussion with a knowledgeable clinician can help you decide if it’s right for you. A few non-hormonal Rx meds may be worth considering for hot flashes, as well.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, nausea, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered. Learn more here.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.







